 ANSI/HL7 V3 CR, R4-2008 HL7 Version 3 Standard: Claims and Reimbursement, Release 4 02/20/2008 |
Content Last Edited: 2009-09-04T22:38:52
6.2 Storyboards
6.3 Application Roles
6.4 Trigger Events
6.5 Refined Message Information Models
6.6 Hierarchical Message Descriptions
6.7 Interactions
Invoice adjudication is the submission of a healthcare Invoice (claim) for adjudication and payment (payment typically occurs subsequent to adjudication, based on a regular payment cycle such as bi-weekly or monthly). The invoice is comprised of a request for payment, costing details that support the payment request and clinical details that support the costing details.
Adjudication results is the mechanism used by an Adjudicator to report how the Invoice was adjudicated, including the rationale for adjusting the Invoice (e.g. over plan maximums). The adjudication results are also known as the explanation of benefits (EOB). The EOB identifier is used on a Payment Advice to assist in the financial reconciliation between intentions to pay (through EOBs) and actual payments (through the Payment Advice).
In addition, Invoice adjudication supports co-ordination of benefits (COB). A COB Package is returned with each EOB, to be included in the submission of the same Invoice to a downstream or subsequent Adjudicator. The COB Package describes a subset of the EOB that is passed from an upstream Adjudicator to the downstream Adjudicator in order for the downstream Adjudicator to properly determine their financial commitment to the Invoice.
State Transition Diagram
|
||||||||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the storyboard discussion in the Version 3 Guide.
To demonstrate the submission for Re-Adjudication of a previously adjudicated and possibly paid Invoice. Re-Adjudication requires the Adjudication Manager to revisit and Re-Adjudicate a previously submitted Invoice.
| Inv Request, Gen | |
| Inv Comp Results Comp, Gen | |
| Inv Comp Results Comp, Gen |
In this scenario, Dr. Bob Bender submits an Invoice with chiropractic health service code 11.12A for an office visit to discuss a patient's diagnosis and treatment for a neck and shoulder injury. The cost of the office visit was $ 45.47. The billing clerk also submitted a claim for 2-lower back x-rays for $123.23 on the same date of service.
The Invoice for the office visit is assessed to 0 (zero) by the provincial insurer because the assessment rule states that when the same practitioner submits a claim for the same patient for the same date of service for an office visit and x-rays for related diagnostic codes, the greater amount of the two services is paid.
Dr. Bender felt there were circumstances that required a manual review of the Adjudication Results. The billing clerk created a Re-Adjudication Invoice for health service code 11.12A that included the following as supporting information:
-
The patient has 2 separate injuries that are being treated; one is a lower back injury and the other is neck and shoulder injury.
Because the doctor sent this as a Re-Adjudication, the claim went to a manual review queue and staff overrode the rule and the chiropractor was paid for the office visit as well.
The optometrist submitted the following items to their patient's extended benefits insurance plan all with the same service date and patient name:
-
Initial visit and assessment
-
1 pair of eyeglasses
-
Eyeglass Adjustment
The payor rejected the third line item indicating payment was refused, as this service is included in the benefit paid for the initial visit and assessment.
The optometrist felt there were circumstances that required a manual review of the Adjudication Results. The billing clerk created a Re-Adjudication Invoice for the eyeglass adjustment including the following explanatory information:
-
Patient has 2 sets of eyeglasses; adjustment was completed on their existing eyeglasses and not related to their new glasses.
Based on the explanatory information, the claim was Re-Adjudicated manually and the full amount paid.
To demonstrate the submission for Re-Adjudication of a previously adjudicated and possibly paid Invoice. Re-Adjudication requires the Adjudication Manager to revisit and Re-Adjudicate a previously submitted Invoice.
| Inv Request, PAccom | |
| Inv Comp Results Comp, PAccom | |
| Inv Comp Results Comp, PAccom |
Adam Everyman arrives at the hospital for a scheduled admission on Day 1, and requests a Semi-private Room. Upon eligibility check the patient discovers a $200 deductible is owed, and it is paid with a credit card. On Day 2, Adam Everyman is transferred to ICU, but is returned to a semi-private room on Day 3. On Day 3 the patient requests a Private Room and is transferred at 9pm. The patient remains in a Private Room until discharge on Day 6.
The hospital submits an Invoice on the discharge day to the insurance company for a 1-night stay in Semi-private and a 3-night stay in Private, including the paid deductible. Two days later the hospital receives the adjudication results from the insurance company. Payment for the Private Room is declined as the Patient recently changed plans with the insurance company and the new plan does not cover Private accommodation.
The hospital requests re-adjudication of the invoice providing documentation to verify that Adam Everyman still had extended coverage at the time the service (Private Room) was provided to him. The change in insurance plans occurred after Adam Eveyman's hospital stay.
The insurance company responded three days later. Adjudication results showed that the full invoiced amount would be paid.
To demonstrate the submission of a Chiro Physio Invoice which includes both Service and Product together
Jack Sprite has been treated by Physio Therapist Nancy Twist for a period of time for a knee weakness and pain. Jack has complained of re-injuring his knee so Nancy has recommended the use of a knee brace to protect against re-injury. Jack obtains written permission from his EHC insurer to get the brace. Nancy makes a custom brace and fits it to Jack at their next treatment session. Nancy submits an Invoice Adjudication Request that charges separately for the time to make the brace, the materials utilized and the fitting session time. These items are submitted as a group of items to be adjudicated together as the insurer will not pay for a brace (ready made or custom) if it is not also fitted by the Physio Therapist. Also, when the cost of time to make a custom brace plus the materials cost of a custom brace exceeds a specified total, only a portion will be paid. Therefore, both items must be adjudicated together.
Jason Mask had pain in his right arch which he presented to his Chiropractor Bill Green at multiple treatment sessions. Bill's treatment included providing Jason with a pair of orthodic inserts. When Bill provided the inserts, he invoiced Jason's EHC insurer for both the treatment session and the inserts in an invoice group to be adjudicated together. The adjudication result included a partial payment of the inserts as it was determined that Jason was receiving regular treatment for the same diagnosis and the condition would be helped by the inserts. The expectation was that Jason would recover with fewer treatments.
To demonstrate how a Generic Invoice is submitted and adjudicated. This storyboard depicts a response where no initial 'identifier' handshake takes place. The only response is the final adjudication result.
| Inv Request, Gen | |
| Inv Comp Results Comp, Gen |
Mr. Adam Everyman strains his back while at work and goes to see his General Practitioner, Dr. F. Family, who determines the patient may benefit from physiotherapy. The doctor's office submits a manual form to HC Payor, Inc. to establish a claim (which is accepted by the Case Manager). They then refer Mr. Everyman to the Early Recovery Clinic for treatment. This physical therapy clinic has an established relationship with HC payor, Inc. and routinely submits Fee for Service Invoices for payment.
HC payor, Inc. has not specifically authorized any services for Mr. Everyman. However, this initial visit is covered under its usual business practices with the Early Recovery Clinic. That is, Invoices for assessments, treatments and reports are accepted by HC payor, Inc. under the conditions of their contract with the Physiotherapy Association when a physician has referred the patient.
When Mr. Everyman arrives at the clinic for his visit, the clerk asks Mr. Everyman for his care card, (for patient identification purposes only) confirms his claim number (# 49349) and that the visit is a result of a work place accident that occurred on June 14, 2001.
Seth Stretcher, a practitioner at the Early Recovery Clinic, sees Mr. Everyman for an initial assessment visit. During his assessment, the practitioner determines that a single treatment visit that includes back exercise, ultrasound and external massage to the back should be sufficient and could be completed during this visit.
At the end of the patient's visit, the clinic's billing clerk arranges to submit an Invoice on his behalf for a single physical therapy visit including assessment and also identifies the 3 therapy procedures provided to the patient:
-
1SJ02YP Exercise therapy, back - using mobility exercise (functional)
-
1SJ07JAAZ Hypothermia, back NEC - using ultrasound device
-
1SJ05JJ Manual therapy, back - using external massage
The clinic's billing system receives a message level 'acknowledgement' from HC Payor, Inc. that the invoice has been received. No other information is exchanged at that time.
Two days later, HC Payor, Inc. sends the final adjudication results and indicated an intent to pay the single line item in full, to the clinic.
Seth Stretcher, a practitioner at the Eraly Recory Clinic, has been treating Mr. Everyman for a back strain that occurred at work and caused him to be away from his job until recovered. During his third visit, the practitioner determines that this treatment and 2 more treatment visits that include stretching, ultrasound and external massage to the back should be enough treatment and Mr. Everyman can return to work next Monday.
At the end of the patient's visit, the clinic's billing clerk prepares a single patient, single line item Invoice for on-line submission to HC Payor, Inc. to request adjudication and payment for the visit. The practice management/billing application in the clinic assigns a unique Invoice number to the Invoice, defaults the Payee for the Invoice to the Early Recovery Clinic, automatically fills in the patient information (Adam Everyman, ID # 592939), patient's insurance coverage which is identified as a HC Payor, Inc. claim number (# 49349). The billing clerk enters a fee code of 19162 for a single physical therapy visit and enters Seth Stretcher as the service Provider.
Upon entry and confirmation of the Invoice, the billing clerk submits the Invoice to HC Payor, Inc. for adjudication and payment.
HC Payor, Inc. responds to the Invoice submission with Adjudication Results, identifying HC Payor's Invoice number and that the single item payment request was adjudicated as an Error and would not be paid. The Adjudication Result reason indicates that the "Invoice item incomplete - missing procedure identification".
Mr. Adam Everyman strains his back while at work and goes to see his General Practitioner, Dr. F. Family, who determines the patient will benefit from physiotherapy. The doctor's office submits a manual form to the HC Payor, Inc. to establish a claim (which is accepted by the Case Manager). They then refer Mr. Everyman to the Eraly Recovery Clinic for physiotherapy treatment. The Early Recovery Clinic has an established relationship with HC Payor, Inc. and routinely submits Fee for Service claims for payment.
HC Payor, Inc. has not specifically authorized any services for Mr. Everyman. However, this initial visit is covered under its usual business practices with the Early Recovery Clinic. That is, claims for assessments, treatments and reports are accepted by HC Payor, Inc. under the conditions of their contract with the Physiotherapy Association, when a physician has referred the patient.
The Early Recovery Clinic has an integrated practice management and billing application. When Mr. Everyman arrives at the clinic for his visit, the clerk asks Mr. Everyman for his care card (for patient identification purposes only) and confirms the HC Payor claim number (# 49349) and that his visit is a result of a work place accident on June 14, 2001.
Seth Stretcher, a practitioner at the Early Recovery Clinic, sees Mr. Everyman for an initial visit and, having determined that further treatment is required, produces a Treatment/Assessment Plan and also provides Return To Work Education. Subsequent treatments are undertaken over the next 3 weeks and at the end of that time, a Treatment/Assessment Visit occurs where it is determined Mr. Everyman can return to work.
At the end of the patient's first visit, the clinic's billing clerk prepares an single patient, multi-line item Invoice for on-line submission to HC Payor, Inc. to request adjudication and payment for the visit, preparation of the treatment/assessment plan and the return to work (RTW) education. The practice management/billing application in the clinic assigns a unique Invoice number to the Invoice, defaults the Payee for the Invoice to the Early Recovery Clinic Inc., automatically fills in the patient information (Adam Everyman, ID # 592939) and the patient's insurance coverage as identified by the HC Payor claim number (# 49349).
The billing clerk enters three services, each with Seth Stretcher as the attending Provider:
-
Initial Visit [Including Assessment] (19160) which included the following procedures:
-
1SJ02YP Exercise therapy, back - using mobility exercise (functional)
-
1SJ07JAAZ Hypothermia, back NEC - using ultrasound device
-
1SJ05JJ Manual therapy, back - using external massage
-
-
1 Treatment/Assessment Plan (19174) (+ EDI Fee),
-
RTW Education (19168) (+ EDI Fee)
Upon entry and confirmation of the Invoice, the billing clerk submits the Invoice to HC Payor, Inc. for adjudication and payment.
HC Payor, Inc. immediately responds to the Invoice submission with Adjudication Results, identifying HC Payor's Invoice number and Adjudication Results for each of the line items billed. Each of the line items billed was approved as submitted and will be paid in full by HC Payor.
Three Chiropractor practitioners at the Bender Clinic share the practice, working from between 3 to 4 days each week. They each see numerous patients every day all receiving a variety of treatments and services. The Bender Clinic bills the provincial insurer at the end of each day for each of the treatments and services provided to their patients that are covered under the provincial insurance plan. Under this plan, patients can receive up to 15 chiropractic visits per calendar year with an additional $ 12.00 user fee per visit. Each of the patient's are requested to pay the $12.00 user fee upon registration, which can then be recovered by the patient from an extended benefit plan, if applicable. At the end of each day, the clinic's billing clerk prepares a multi-patient, multi-line item Invoice for the provincial insurer, requesting on-line adjudication and payment for the chiropractic services provided that day.
The billing clerk enters the patient, insurance and diagnosis information. If each of the services for a patient were performed by the same chiropractor, the Provider's role in the service, their name and identifier is entered.
Each of the services provided to a patient are identified. The services are entered using the appropriate insurer product/service code and the associated charge is automatically brought forward from the product/service code master file.
When all services and patients are entered, the billing application creates an Invoice and assigns a unique Invoice number to the Invoice and defaults the Payee to the Bender Clinic. The billing clerk enters her name and telephone number as the Billing Contact Person.
When the Invoice is complete and has been reviewed, the billing clerk submits the Invoice to the provincial insurer for adjudication and payment.
The provincial insurer responds immediately with Adjudication Results identifying approved, approved with adjustments and rejected items. Reasons for partial payment and rejection are noted so that the billing clerk can make appropriate modifications for re-submission or payment re-direction.
A Psychologist practitioner at the West One Clinic works with groups of patients for certain therapies. They each see 3 or 4 patients in a treatment session. The West One Clinic bills the Workers Compensation (or other) insurer for each of the treatment sessions. Each of the patients may have a separate claim number that identifies their coverage or the group of patients may be covered under one insurance. At the end of each day, the clinic's billing clerk prepares a multi-patient, single item Invoice for the insurer, requesting on-line adjudication and payment for the Psychologist's services provided that day. The billing clerk enters each patient's, insurance (in this case claim number) and diagnosis information. The service for the patients (in this instance) was performed by the one Psychologist, the Provider's role in the service, their name and identifier is entered. A separate Billable Act set of information is created for each patient and a separate set of insurance and covered party information also created. The session service provided to the patients is identified. The service is entered using the appropriate insurer product/service code and the associated charge is automatically brought forward from the product/service code master file. This creates one invoice item for the treatment session. When the service and patients are entered, the billing application creates an Invoice and assigns a unique Invoice number to the Invoice and defaults the Payee to the West One Clinic. The billing clerk enters her name and telephone number as the Billing Contact Person. When the Invoice is complete and has been reviewed, the billing clerk submits the Invoice to the insurer for adjudication and payment. The insurer responds immediately with Adjudication Results identifying approved, approved with adjustments and rejected items. Reasons for partial payment and rejection are noted so that the billing clerk can make appropriate modifications for re-submission or payment re-direction.
To demonstrate how a Generic Invoice is submitted with adjudication including Coordination of Benefits. An Invoice can represent a single billable line item, multiple billable line items for 1 patient and daily billing (multiple patients in 1 Invoice, each having 1 or more billable line items).
| Inv Request, Gen | |
| Inv Comp Results Comp, Gen | |
| Inv Request, Gen | |
| Inv Comp Results Comp, Gen |
Adam Everyman is covered by two insurance plans that provide benefits coverage for extended chiropractic practitioner fees. The primary plan pays up to 80% of the service fee and the secondary plan pays up to 50% of the service fee.
Dr. Bender practices in a clinic with 3 other chiropractors. Each of the practitioners share the services of the billing clerk who performs all patient registration, clinical and billing functions on the integrated practice management and billing application.
Adam Everyman, who Dr. Bender treats on a regular basis for a previous back injury, presents at Dr. Bender's office for a subsequent visit. The clerk searches for the patient in the practice management system using the patients' last name, first name and date of birth. The clerk confirms the patient's demographic information and insurance coverage. Lee Smith is currently insured for primary extended chiropractic coverage under HC Payor's, Inc. unionized employer group plan (group # 49324 and policy # 234-794-9493) and U Are Insured's individual plan (group # 99999 and policy # 14372). Mr. Everyman is also covered under a government sponsored insurance plan for chiropractic office, home, institutional or emergency room services.
During the single session office visit, Dr. Bender determines that a lower back x-ray is required to determine healing progress and that this service is covered under the patient's extended benefits plan. Upon completion of the office visit and delivery of the lower back x-ray to Adam Everyman, the billing clerk creates a single line item Invoice to request adjudication and payment for the x-ray service to the extended benefit insurer. (Note: the clerk also creates a separate Invoice to the government sponsored insurance plan for the office visit charge).
The billing module assigns a unique Invoice number (# 1233) to the new Invoice, HC Payor, Inc. as the Payor and the Payee information defaults to Dr. Bender Inc. The billing clerk enters her name and number as the contact for the Invoice, and enters Dr. Bender (ID 4758934) as the service Provider. The patient information (ID # 720134071, Adam Everyman, DOB = 1945 Feb. 12) and primary and secondary insurance identifiers, name and coordination of benefit priority are automatically brought forward from the registration module. The patient's diagnosis of backache, unspecified, (724.5) is also brought forward from the clinical module and entered on the Invoice.
The billing clerk enters a product/service code of 47537 to identify the lower back x-ray and a quantity of 1. The billing application automatically creates a unique product/service line number, defaults the service date to today's date and pulls the unit cost ($50.00) and description from the product/service code master file. The application calculates the total cost of the service and billed amount to $50.00 (as there are no Provider adjustments for this line item).
The billing clerk reviews and submits the completed Invoice to HC Payor, Inc..
Two days later, HC Payor, Inc. processes the Invoice and issues Adjudication Results to the Provider indicating an approved as amended adjudicated/paid amount of $40.00 (reason code: benefit maximum reached).
The Provider application processes the Adjudication Results and reports that there is still an outstanding balance on the Invoice and that the secondary Payor accepts coordination of benefits.
The billing clerk assembles a new single line item Invoice, bringing forward the information from Invoice # 1233, including the unmodified Adjudication Results details from HC Payor, Inc. The billing clerk changes the Payor to U Are Insured and submits the Invoice.
One day after receiving the invoice, U Are Unsured processes the Invoice and issues Adjudication Results for approval and subsequent payment of $10.00 to the Provider.
The Provider is paid the appropriate amount for the service by each of the Payors in the next pay period.
Three Chiropractor practitioners at the Bender Clinic share a practice working from between 3 to 4 days each week. They each see numerous patients every day all receiving a variety of treatments and services. The Bender Clinic bills insurers at the end of each day for each of the treatments and services provided to their patients that are covered under their respective insurance plans.
Extended Chiropractic practitioner benefits are generally covered by a primary plan that pays up to 80% of the service fee and a secondary plan that pays up to 50% of the service fee.
At the end of each day, the clinic's billing clerk prepares a multi-patient, multi-line item Invoice for the primary insurer, requesting on-line adjudication and payment for the chiropractic services provided that day.
The billing clerk enters the patient, insurance and diagnosis information. If each of the services for a patient were performed by the same chiropractor, the Provider's role in the service, their name and identifier is entered.
Each of the services provided to a patient are identified. The services are entered using the appropriate insurer product/service code and the associated charge is automatically brought forward from the product/service code master file.
When all services and patients are entered, the billing application creates an Invoice and assigns a unique Invoice number to the Invoice and defaults the Payee to the Bender Clinic. The billing clerk enters her name and telephone number as the Billing Contact Person.
When the Invoice is complete and has been reviewed, the billing clerk submits the Invoice to the primary insurer, for adjudication and payment.
The primary insurer responds with Adjudication Results identifying approved, approved with adjustments and rejected items. Reasons for partial payment and rejection are noted so that the billing clerk can make appropriate modifications for re-submission or payment re-direction.
The Provider application processes the Adjudication Results and reports that there are still outstanding balances on the Invoice for some of the patients and that the patients secondary Payors accepts coordination of benefits.
The billing clerk assembles new Invoices, containing the patients for each secondary payor, bringing forward the information from the original Invoice, including the unmodified Adjudication Result details from the primary payor. The billing clerk changes the Payor to the appropriate secondary payor and submits the Invoices.
The secondary payors process the Invoices and issue Adjudication Results for approval and subsequent payment to the Provider.
The Provider is paid the appropriate amount for the service by each of the primary and secondary Payors in the next pay period.
To demonstrate the submission of a Pharmacy invoice adjudication request, the communication of the adjudication results and the subsequent payment.
In this scenario, only final adjudication results are communicated. No initial or pre-processing information is provided to the Adjudication Requestor.
| Inv Request, Rx | |
| Inv Comp Results Comp, Rx |
On January 7,2002, Adam Everyman brings his prescription for 30 Zantac 300mg. to Good Neighbor Pharmacy. Mr. Everyman has never had prescriptions filled at this pharmacy before. Susan Script, the pharmacist, asks Mr. Everyman for his demographic information in order that he may create a patient profile for Mr. Everyman. This includes information on any drug allergies and existing medical conditions. Susan then asks Mr. Everyman if he has a drug plan. Mr. Everyman gives Susan his Provincial Drug plan card. Susan asks Mr. Everyman his date of birth and enters this along with his Provincial Health Card numbers. Susan knows that the provincial plan will only pay the drug cost for the equivalent generic brand. Susan determines from the formulary that the provincial plan will pay 0.7787 cents per tablet for a total drug cost of $23.61. The total drug cost for brand name Zantac would be $61.86. Susan explains to Mr. Everyman that the provincial plan will only pay the cost of the generic equivalent drug and if he wishes to have the brand name product, he will have to pay the difference in cost of $38.25 in addition to the co-pay, which is equivalent to the professional fee of $8.90. Mr. Everyman decides to take the generic equivalent.
Susan enters the required information into the pharmacy desktop computer system. The system calculates the drug cost to be $23.61 and it applies a professional fee of $8.90. The required prescription information and costs, along with Mr. Everyman's name and Provincial Health Card numbers are electronically transmitted to the provincial plan adjudicator. The information is processed through the adjudicator's computer system and in five seconds or less, a response is transmitted back to Good Neighbor Pharmacy. The response indicates that the drug cost will be paid in full by the provincial plan and that Mr. Everyman will owe a co-pay or $8.90
Susan, with the assistance of his pharmacy technician, completes filling the prescription. Susan presents the filled prescription to Mr. Everyman and advises him of the proper use of the drug, as well as information on relevant precautions and potential side effects. Mr. Everyman pays Susan the $8.90 co-pay and leaves the pharmacy with his prescription.
Throughout the rest of the day (January 7, 2002), the staff at Good Neighbor Pharmacy submits additional prescription invoices for various patients. Each of these invoices is Adjudicated as Submitted, Adjudicated with Adjustments or Adjudicated as Refuse. In addition, Invoice Cancellation requests may also be submitted.
At the end of the business day, Susan transmits a query to the adjudicator of the Provincial Plan requesting an Account Summary of all transactions occurring between the Provincial Plan and Good Neighbor Pharmacy that day. The adjudicator creates a Payment Advice giving an aggregate total dollar amount that will be deposited in a bank account specified on file for Good Neighbor Pharmacy. The Payment Advice also details each adjudicated invoice, including those invoices that were Adjudicated as Submitted, Adjudicated with Adjustments (i.e. not paid the same as submitted and could be paid as $0) and Adjudicated as Refuse (effectively, paid as $0). The Payment Advice also includes information on any changes as a result of Cancellations. The Payment Advice is transmitted to Good Neighbor Pharmacy.
A young man, John Wanderer, moves to a new city in Ontario, expecting that he will find employment. Unfortunately, work is not available and he finds that he must access the city's social services department for assistance. The social services department agrees to provide temporary support, including temporary drug benefits as John is on chronic medications. They issue John a paper drug card which is valid until the end of the month. This office is not on-line in real time with the provincial drug benefit program which will adjudicate the claims, so it will take some time for the information on John's drug benefit coverage to be activated in the provincial system.
John proceeds to a local pharmacy to have a prescription dispensed. He provides his demographic data along with his prescription and his new drug benefit card. The appropriate data is entered into the Pharmacy Management System, including the expiry date indicated on the drug benefit card and the electronic invoice is transmitted to the provincial drug plan adjudicator. John's drug benefit coverage has not yet been activated in the adjudicator's system so the payment request is refused as John is believed to be ineligible under the plan. As the pharmacist has a valid drug benefit card in hand, they resubmit the invoice with a good faith override and the pharmacist's identifier. The good faith override establishes coverage for John in the provincial system through to the expiry date supplied. Subsequent invoices for medications for John during that time period will not require (do not allow) the good faith override with the invoice.
To demonstrate how a Pharmacy Invoice is created, submitted and adjudicated. This storyboard depicts a response where no initial 'identifier' handshake takes place. The only response is the final adjudication result.
| Inv Request, Rx | |
| Inv Comp Results Comp, Rx |
On January 7,2002, Adam Everyman brings his prescription for 30 Zantac 300mg. to Good Neighbor Pharmacy. Mr. Everyman has never had prescriptions filled at this pharmacy before. Susan Script, the pharmacist, asks Mr. Everyman for his demographic information in order that he may create a patient profile for Mr. Everyman. This includes information on any drug allergies and existing medical conditions. Susan then asks Mr. Everyman if he has a drug plan. Mr. Everyman gives Susan his Provincial Drug plan card. Susan asks Mr. Everyman his date of birth and enters this along with his Provincial Health Card numbers. Susan knows that the provincial plan will only pay the drug cost for the equivalent generic brand. Susan determines from the formulary that the provincial plan will pay 0.7787 cents per tablet for a total drug cost of $23.61. The total drug cost for brand name Zantac would be $61.86. Susan explains to Mr. Everyman that the provincial plan will only pay the cost of the generic equivalent drug and if he wishes to have the brand name product, he will have to pay the difference in cost of $38.25 in addition to the co-pay, which is equivalent to the professional fee of $8.90. Mr. Everyman decides to take the generic equivalent.
Susan enters the required information into his pharmacy desktop computer system. The system calculates the drug cost to be $23.61 and it applies a professional fee of $8.90. The required prescription information and costs, along with Mr. Everyman's name and Provincial Health Card numbers are electronically transmitted to the provincial plan adjudicator. The information is processed through the adjudicator's computer system and in five seconds or less, a response is transmitted back to Good neighbor Pharmacy. The response indicates that the drug cost will be paid in full by the provincial plan and that Mr. Everyman will owe a co-pay or $8.90
Susan, with the assistance of his pharmacy technician, completes filling the prescription. Susan presents the filled prescription to Mr. Everyman and advises him of the proper use of the drug, as well as information on relevant precautions and potential side effects. Mr. Everyman pays Susan the $8.90 co-pay and leaves the pharmacy with his prescription.
Adam Everyman receives a prescription from his physician, Dr.F. Family, for Zocor 20 mg to treat his elevated cholesterol. The prescription calls for 30 tablets to be dispensed, with the directions to read: Take one tablet daily at bedtime.
Mr. Everyman presents the prescription to Ms. Script, the pharmacist at the the Good Neighbor Pharmacy. Mr. Everyman is a regular patient at Good Neighbor Pharmacy and his demographic and third party drug plan information is all on file in the pharmacy prescription computer system.
Ms. Script enters the pertinent information from the new prescription into the Good Neighbor Pharmacy system and then transmits the information as an real time Invoice to Mr. Everyman's third party drug plan adjudicator. The data is processed through the computer system at the third party adjudicator. It is determined that Mr. Everyman is eligible to receive benefits, that this drug is a benefit under Mr. Everyman's plan and that the quantity of the prescription falls within the drug plan guidelines. The third party adjudicator sends a message to the prescription system at the Good Neighbor Pharmacy, stating that they intend to pay for the claim for Mr. Everyman as submitted.
Mr. Adam Everyman, who has had a mechanical prosthetic heart value for 6 months, visits his doctor for routine assessment of his INR. His current dose of warfarin is 3mg daily, but as a consequence of this latest INR result, Dr. Patricia Primary wants to increase the dose to 4mg on one day, 5mg on the alternate day. Having discussed this with Mr. Everyman, and being sure that he understands exactly what he is going to do, and how he will achieve this, Dr Primary writes him a prescription listing three products, so that he has the most convenient dosage options available to him:
-
Rx: Warfarin 1mg tablets (bs17. y01lx), mitte 100, sig: ut dict
-
Rx: Warfarin 3mg tablets (bs18. y01ly), mitte 100, sig: ut dict
-
Rx: Warfarin 5mg tablets (bs19. y01lz), mitte 100, sig: ut dict
Whilst with the doctor, Mr. Everyman mentions to Dr. Primary that he has been suffering from a contact dermatitis on his hands that he has been unable to treat successfully using the hydrocortisone cream that he was able to purchase from his local pharmacy. Dr. Primary suggests that a short course of a stronger steroid might conquer the problem, and adds an order for this to the prescription:
-
Rx: Betametasone 0.1% ointment (m48r. y03AA), mitte 30g, sig: apply bd
Mr. Everyman takes his prescription for the three items to the pharmacist at Good Neighbour Pharmacy for dispensing. Mr. Everyman does not fulfil any of the criteria for exception from NHS Prescription Charges, and therefore should pay a charge for each item on the prescription. However, NHS Regulations state that when a single prescription (form) contains items of the same active ingredients and formulation, but of different strengths, only one Prescription Charge is payable by the patient to cover all the strengths of products supplied, but that the pharmacist may claim reimbursement of a professional fee for each individual item supplied. Consequently, Mr. Everyman pays only two Prescription Charges to the Good Neighbour Pharmacy when he receives his four dispensed items, but Pharmacist Susan Script requests reimbursement of professional fees for all four dispensed items, annotating the prescription with a two fees, two no-charges record. An invoice is submitted and full payment is received.
Adam Everyman receives a prescription from his physician, Dr. F. Family, for Zocor 20 mg to treat his elevated cholesterol. The prescription calls for 100 tablets to be dispensed, with the directions to read:Take one tablet daily at bedtime.
Mr. Everyman presents the prescription to Ms. Script, the pharmacist at the Good neighbor Pharmacy. Mr. Everyman is a new patient at Good neighbor Pharmacy. Mr. Script obtains all pertinent demographic and third party drug plan information from Mr. Everyman and enters it into the Good Neighbor Pharmacy prescription computer system.
Ms. Script then enters the pertinent information from the new prescription into the Good Neighbor Pharmacy system and then transmits the information as an real time Invoice to Mr. Everymans third party drug plan adjudicator. The data is processed through the computer system at the third party adjudicator. The computer determines that while Mr. Everyman's name and third party information is a match, the birth date supplied does not match the one they have on file. The third party adjudicator sends a message to the prescription system at Good Neighbor Pharmacy, stating that they will not pay for the Invoice, as there is a birth date error.
Ms. Script speaks to Mr. Everyman and finds that he has transposed two numbers when entering Mr. Everyman's birth date into his pharmacy system. Ms. Script changes the birth date information in the pharmacy system and then resubmits the Invoice with a new identification number to the third party adjudicator. This time, there is a match on all of Mr. Everyman's information, the drug is an eligible benefit and the quantity falls within the plan limits. A message is sent from the third party adjudicator computer to the store computer stating that they intend to pay for the resubmitted Invoice.
Following a series of visits with his physician, Dr. F. Family, Mr. Adam Everyman receives three prescriptions. Two of the prescriptions, Cozaar 50 mg once daily, dispense 30 tablets and Hydrochlorothiazide 25 mg once daily, dispense 30 tablets, have been prescribed to treat his high blood pressure. Zocor 20 mg once daily, dispense 30 tablets has been prescribed to treat his elevated cholesterol.
Mr. Everyman presents the prescriptions to Ms. Script, the pharmacist at the Good Neighbor Pharmacy. Mr. Everyman is a regular patient at the Good Neighbor Pharmacy and his demographic and third party drug plan information is all on file in the pharmacy prescription computer system.
Ms. Script enters the pertinent information from the each prescription into the Good Neighbor Pharmacy system. The three claims are packaged by the prescription computer system and transmitted as a single real time message to Mr. Everyman's third party drug plan adjudicator. The data for each individual line item is processed through the computer system at the third party adjudicator. It is determined that Mr. Everyman is eligible to receive benefits, that these three drugs are all benefits under Mr. Everyman's plan and that the quantity of each prescription falls within the drug plan guidelines. The third party adjudicator sends a message to the prescription system at Good Neighborl Pharmacy, stating that they intend to pay for the three line items for Mr. Everyman as submitted.
To demonstrate how a Pharmacy Invoice is submitted and adjudicated including Coordination of Benefits. An Invoice can represent a single billable line item or multiple billable line items.
| Inv Request, Rx | |
| Inv Comp Results Comp, Rx | |
| Inv Request, Rx | |
| Inv Comp Results Comp, Rx |
On January 7, 2002 Adam Everyman brings his new prescription into Good Neighbor Pharmacy. Mr. Everyman has been getting his prescriptions here for almost two years. Mr. Everyman is a senior and has his medications paid for under the provincial plan. His new Rx is written for 90 Ditropan. The pharmacist, Susan Script, after consulting with Mr. Everyman fills the prescription with the generic Oxybutynin. Mr. Everyman does not want to pay the cost difference of the brand and generic drug. Susan determines the cost of the generic drug will be $23.37. The professional fee will be $8.90. This is the maximum fee allowed by the provincial plan. There is a co-pay of $8.90, which is equal to the fee.
Susan fills the prescription and gives Mr. Everyman the receipt indicating he has an $8.90 co-pay.
Mr. Everyman advises Susan that his wife is a teacher and she has a drug plan. He suggests her plan will cover any amount on his prescriptions not covered by the provincial plan. Carol records all the pertinent data relating to the second payor on Mr. Everyman's patient profile. Susan advises Mr. Everyman that in order to submit the residual amount to the second payor, she must include the amount paid by the primary payor, in this case, the provincial plan. Since the provincial plan is not real-time adjudication, Susan suggests to Mr. Everyman that he pay the co-pay and retain his receipt for manual submission to his wife's plan. Mr. Everyman does not want to submit a manual receipt. Since he is a good customer, Susan offers to submit the claim to the second payor once she has received the remittance advice from the provincial plan.
Carol submits the claim to the provincial plan.
On January 21, 2002, Good Neighbor Pharmacy receives the remittance advice from the provincial plan. Mr. Everyman's prescription has been paid in full with the exception of the $8.90 co-pay.
That same day, Susan submits an invoice to the secondary payor along with the required COB information.
On January 30, 2002, Susan receives a remittance from the second payor with full coverage of the $8.90 co-pay.
Mr. Everyman has been getting his prescriptions filled at a local pharmacy for many years. His employer has covered his prescriptions under their pay-direct prescription drug plan. The drug plan is very liberal when it comes to coverage and most items are covered as a plan benefit. The great majority of the time, prescriptions are electronically adjudicated without any problems.
Today, August 08, 2001, Mr. Everyman presents a new prescription for Lipitor, a cholesterol-lowering agent (this is a continuation of ongoing therapy). The pharmacy processes the new prescription in the usual manner and transmits the Invoice to the adjudicator as indicated on the patient record as the primary plan.
This time, the adjudicator's real time response indicates that the prescription is rejected with zero payment. The explanation received on the adjudication response indicates: Patient Covered By Other Plan.
The Pharmacist asks Mr. Everyman if their plan has changed. Mr. Everyman replies that to his best knowledge, nothing has changed. The pharmacy calls the adjudicator's Help Desk to query why this Invoice was rejected and inquires to whom the Invoice should be directed?
The Provider Help Desk does not have the information about the identity of the new Payor. Upon some further investigation it was discovered that Mr. Everyman had turned 65 years of age 3 weeks ago. According to the rules of Mr. Everyman's employer drug plan, the primary Payor now becomes the provincial government.
The Provincial Health Number is obtained from the patient and the provincial government is set up as the primary Payor. The secondary Payor will now be the patient's employer plan. Any residual amounts and items not covered under the government public plan will be sent to the secondary plan.
The prescription is submitted to the provincial drug plan and successfully paid except for $25.00. That amount is the province's maximum allowable amount per prescription deductible. The $25.00 is now submitted to the Mr. Everymans' employer plan with the required Coordination Of Benefits information, indicating how much was paid by the provincial plan. The pharmacy now receives full payment for the $ 25.00 residual amount.
To demonstrate how a Preferred Accommodation Invoice is submitted and adjudicated. This scenario includes patients' requests for a private or semi-private room for part or all of a hospital stay.
| Inv Request, PAccom | |
| Inv Comp Results Comp, PAccom |
Eve Everywoman arrives in the Emergency department accompanied by her mother. Ms. Everywoman is asleep, and her mother answers the questions of the Admission Clerk.
Upon request, the patient is admitted to a Semi-private Room. Ms. Everywoman is discharged on Day 3. The hospital submits an Invoice to the insurance company. Two days later the hospital is informed by the insurance company that the Invoice is denied because only the insured can request a preferred accommodation room.
The hospital subsequently bills Ms Everywoman for 2-nights stay in the semi-private room.
Eve Everywoman arrives by ambulance and is treated in the Emergency department. She is unconscious and unable to answer simple questions. Ms. Everywoman is treated and admitted to a Ward bed for observation. On Day 2 the physician wants to isolate the patient, and transfers her to a Private Room. On Day 3 the admitting department completes the Admission record and learns that Ms. Everywoman has insurance and has requested a Private Room. She remains in the Private Room until discharge.
The hospital does not bill the insurance company for a private room as it was deemed to be medically necessary.
Adam Everyman arrives at the hospital for a scheduled admission on Day 1. At the time of admission he requests a Private Room, and provides his insurance information. A Private Room is available, and he is admitted promptly.
Upon discharge on Day 3, the hospital arranges to submit an Invoice on his behalf for 2-nights Preferred Accommodation at the Private rate of $240 per night.
The next day, the insurance carrier remits the coverage for 2-nights less a $50 co-pay for a total of $190. The hospital applies the amount to the account, and sends a bill to Patient Smith for the $50 co-pay.
Adam Everyman arrives at the hospital for a scheduled admission on Day 1, and requests a Semi-private Room. Upon eligibility check the patient discovers a $200 deductible is owed, and it is paid with a credit card. On Day 2, Mr. Everyman is transferred to ICU, but is returned to a semi-private room on Day 3. On Day 3 the patient requests a Private Room and is transferred at 9pm. The patient remains in a Private Room until discharge on Day 6.
The hospital submits an Invoice on the discharge day to the insurance company for a 1-night stay in Semi-private and a 3-night stay in Private. Two days later the hospital receives the adjudication results from the insurance company. The insurance company will pay the full invoiced amount, less the paid deductible.
To demonstrate how a Preferred Accommodation Invoice is submitted and adjudicated with Coordination of Benefits. An Invoice can represent a single billable line item or multiple billable line items.
| Inv Request, PAccom | |
| Inv Comp Results Comp, PAccom | |
| Inv Request, PAccom | |
| Inv Comp Results Comp, PAccom |
Eve Everywoman is covered by two insurance plans that provide extended benefits coverage. The primary plan, HC Payor Inc., pays up to 80% of the service fee and the secondary plan pays up to 50% of the service fee. Ms. Everywoman requires a hip replacement.
Ms. Everywoman arrives at the hospital for a scheduled admission on Day 1. At the time of admission she requests a Private Room, and provides her insurance information for both plans. A Private Room is available, and she is admitted promptly.
Upon discharge on Day 3, the hospital arranges to submit an Invoice on her behalf for 2-nights Preferred Accommodation at the Private rate of $200 per night in addition to the hip replacement surgery fees. The invoice includes primary and secondary plan identifiers as well as patient, provider and service information. The invoice (#1238) is sent to the primary insurance plan, HC Payor Inc..
Two days later, HC Payor processes the Invoice and issues Adjudication Results to the hospital indicating the results for each billable item. The hip replacement was fully covered but only $200 of the $400 Preferred Accommodation fee was paid. (Reason code: benefit maximum reached).
The hospital application processes each of the Adjudication Results against what was billed and reports that there is still an outstanding balance and that the secondary Payor accepts coordination of benefits. The billing clerk assembles a new Invoice, bringing forward the information from Invoice # 1238 as well as each of the line items, including each of the unmodified Adjudication Results details from HC Payor Inc.. The billing clerk changes the Payor to Uare Insured Inc. and submits the Invoice.
Uare Insured Inc. processes the Invoice one day after receiving it and issues Adjudication Results for approval and subsequent payment of the balance of the invoice.
To demonstrate how a Generic Invoice is submitted, adjudicated and subsequently revised by the Invoice Manager.
| Inv Request, Init/Comp, Gen | |
| Inv Comp Results Comp, Gen | |
| Pre-Det Request, Gen |
On September 23, 2001, See Straight Opticians transmitted an Invoice for a pair of eyeglasses for a total of $834.56. The process was successful and Adjudication Results indicating payment intent of $834.56 were transmitted back to the Optician by the Payor.
This particular Payor employs a Next Day audit program as part of its service offering to its insurance company customers. On September 24, 2001, the Invoice noted above is included in the Next Day audit report. Because this Payor selects all Invoices over $500 for further review, this Invoice is copied from the report and placed onto an audit sheet. The auditor requires further information from the Provider in order to validate the Invoice. A fax form is filled out by the auditor and forwarded to the Provider with a statement that if the information is not forwarded back within 14 days, the Invoice will be reversed.
On October 9, 2001, the auditor reviews the files and notices that a fax form response has not yet been received from the Provider validating the Invoice that was originally processed on September 23, 2001. A revised adjudication form is completed and forwarded to claims processing by the auditor. The claims processor processes the revised adjudication form from the auditor, and reverses the previous adjudication results.
Since this reversal occurred outside of the regular payment cycle, the $834.56 will be deducted from future payments and will be noted as a debit on the Provider's subsequent Payment Advice until the full amount has been recovered.
To demonstrate how a Generic Invoice is created, submitted and adjudicated. An Invoice can represent a single billable line item, multiple billable line items for 1 patient and daily billing (multiple patients in 1 Invoice, each having 1 or more billable line items).
This storyboard also depicts delayed adjudication with an initial response. The initial response exchanges Adjudication Manager identifiers and pre-processing information. Full Adjudication Results are created at a later point in time. Delayed infers that the responses will not be immediate and may lag a request by a period of time (perhaps one or more days).
| Inv Request, Init/Comp, Gen | |
| Inv Init Results Init/Comp, Gen | |
| Inv Comp Results Init/Comp, Gen |
Mr. Adam Eveyman strains his back while at work and goes to see his Family Practitioner, Dr. Fay Family, who determines the patient may benefit from physiotherapy. The doctor's office submits a manual form to HC Payor, Inc. to establish a claim (which is accepted by the Case Manager). They then refer Mr. Everyman to the Early Recovery Clinic for physiotherapy treatment. The clinic has an established relationship with the HC Payor, Inc. and routinely submits Fee for Service Invoices for payment.
HC Payor Inc. has not specifically authorized any services for Mr. Everyman However, this initial visit is covered under its usual business practices with the clinic. That is, Invoices for assessments, treatments and reports are accepted by HC Payor, Inc. under the conditions of their contract with the Physiotherapy Association when a physician has referred the patient.
When Mr. Everyman arrives at the clinic for his visit, the clerk asks Mr. Everyman for his care card, (for patient identification purposes only) confirms his HC Payor, Inc. claim number (# 49349) and that the visit is a result of a work place accident that occurred on June 14, 2001.
Seth Stretcher, a practitioner at the clinic, sees Mr. Everyman for an initial assessment visit. During his assessment, the practitioner determines that a single treatment visit that includes back exercise, ultrasound and external massage to the back should be sufficient and could be completed during this visit.
At the end of the patient's visit, the clinic's billing clerk arranges to submit an Invoice on his behalf for a single physical therapy visit including assessment and also identifies the 3 therapy procedures provided to the patient:
-
1SJ02YP Exercise therapy, back - using mobility exercise (functional)
-
1SJ07JAAZ Hypothermia, back NEC - using ultrasound device
-
1SJ05JJ Manual therapy, back - using external massage
The clinic's billing system receives an initial response from HC Payor Inc. that includes pre-processing information and adjudication related identifiers. The final adjudication results is sent by the payor three days later and includes all adjudication results and resulting payment intent information.
Seth Stretcher, a practitioner at the Early Recovery Clinic, has been treating Mr. Everyman for a back strain that occurred at work and caused him to be away from his job until recovered. During his third visit, the practitioner determines that this treatment and 2 more treatment visits that include stretching, ultrasound and external massage to the back should be enough treatment and Mr. Everyman can return to work next Monday.
At the end of the patient's visit, the clinic's billing clerk arranges to submit an Invoice on his behalf for the visit. The billing clerk submits the invoice for the five treatments using a fee code of 19162 for each physical therapy visit.
HC Payor Inc. receives the invoice and initiates pre-processing. During pre-processing, HC Payor, Inc. determines that the patient has already received the maximum number of covered physical therapy visits for the year. A Coverage Extension is required to extend coverage. HC Payor Inc. returns an error message to the clinic and denies payment.
To demonstrate the submission of a Pharmacy invoice adjudication request, the communication of the adjudication results and the subsequent payment.
In this scenario, the Adjudication Manager sends pre-processing (initial) results, which are followed at a later point in time by the final adjudication results.
| Inv Request, Init/Comp, Rx | |
| Inv Init Results Init/Comp, Rx | |
| Inv Comp Results Init/Comp, Rx | |
| Pymt Adv Detail Results, Gen |
Good Neighbor Pharmacy is a small volume pharmacy. As a result, the pharmacy is unable to purchase its pharmaceutical items direct from the manufacturer and must rely on a wholesaler. This unfortunately has resulted in the store purchasing some pharmaceutical items at a cost that is greater than what most of the payors will allow. Whenever these items are billed to the payors, they are billed as Cost to Operator invoices.
On January 26, 2002, the pharmacist receives a prescription for one of these items. The prescription information is entered into the practice management system and the prescription is processed. As the invoice is being prepared, the pharmacist enters into the appropriate field in his system the code that signifies that this invoice is a Cost to Operator invoice. The drug cost noted on this invoice is the store's actual acquisition cost, which exceeds the payor's allowable cost. The invoice is completed and transmitted to the payor.
Upon recognizing the Cost to Operator code on this inbound invoice, the payor system automatically places the Invoice into a queue for manual review. The invoice undergoes some preliminary adjudication and a response is forwarded to the pharmacy indicating the following:
-
The patient is eligible.
-
The drug is eligible.
-
Before final adjudication can occur, manual follow up is required.
-
Final adjudication results will be forwarded within 24 hours.
Upon receipt of this response, the pharmacy's practice management system pends this invoice and waits for the final response. Meanwhile the pharmacist is aware that he will be paid, however he doesn't know how much yet.
On January 27, 2002, a claims adjudicator pulls the invoice from the queue and attempts to follow up with the suppliers of the pharmaceutical product to verify the cost being billed. As part of their internal process, the claims adjudicator will notify the Drug Identification Number Database if the cost of a particular item needs to be modified in the database. In this particular case, this does not occur as the item can be purchased from other suppliers at a lower cost to the pharmacy. However, the claims adjudicator has been able to verify that the cost submitted is correct, is comfortable with the situation and enters the appropriate information into the system authorizing the payment as submitted. The system then generates a final adjudication response to the invoice informing the pharmacy that this invoice will be paid in full. Upon receipt of the final response, the pharmacy's practice management system links the invoice to the initial response and the final response, and completes the invoice process.
On the day that the Invoice has completed adjudication processing (January 27, 2002), the payor has adjudicated a total of 20 Invoices for Good Neighbor Pharmacy. Each of these Invoices is adjudicated as either Refused, Paid with Adjustment or Paid as Submitted.
At the end of the day (January 27, 2002), the payor summarizes all paid Invoices for each of its Payees (as designated on the Invoice). In this case, the Good Neighbor Pharmacy has designated that all payments be directed to their own Pharmacy. The payor creates a Payment Advice giving an aggregate total dollar amount that will be deposited in a bank account specified on file for Good Neighbor Pharmacy. The Payment Advice also details each paid item, including those Invoices that were Refused (effectively, paid as $0), Paid with Adjustment (i.e. not the same as submitted and could also be paid as $0) and Paid as Submitted. The Payment Advice is sent to Good Neighbor Pharmacy (acting as a Payment Tracker).
To demonstrate how a Pharmacy Invoice is created and submitted. An Invoice can represent a single billable line item or multiple billable line items.
This storyboard also depicts delayed adjudication with an initial response. The initial response exchanges Adjudication Manager identifiers and pre-processing information. Full Adjudication Results are created at a later point in time. Delayed infers that the responses will not be immediate and may lag a request by a period of time (perhaps one or more days).
| Inv Request, Init/Comp, Rx | |
| Inv Init Results Init/Comp, Rx | |
| Inv Comp Results Init/Comp, Rx |
Good Neighbor Pharmacy is a small volume pharmacy. As a result, the pharmacy is unable to purchase its pharmaceutical items direct from the manufacturer and must rely on a wholesaler. This unfortunately has resulted in the store purchasing some pharmaceutical items at a cost that is greater than what most of the payors will allow. Whenever these items are billed to the payors, they are billed as Cost to Operator invoices.
On January 26, 2002, the pharmacist receives a prescription for one of these items. The prescription information is entered into the practice management system and the prescription is processed. As the invoice is being prepared, the pharmacist enters into the appropriate field in his system the code that signifies that this invoice is a Cost to Operator invoice. The drug cost noted on this invoice is the store's actual acquisition cost, which exceeds the payor's allowable cost. The invoice is completed and transmitted to the payor.
Upon recognizing the Cost to Operator code on this inbound invoice, the payor system automatically changes the role from Real time to Delayed Initial Response. The rationale being that manual intervention is required prior to final adjudication on these types of invoices. The invoice undergoes some preliminary adjudication and a response is forwarded to the pharmacy indicating the following:
-
The patient is eligible.
-
The drug is eligible.
-
Before final adjudication can occur, manual follow up is required.
-
Final adjudication results will be forwarded within 24 hours.
Upon receipt of this response, the pharmacy's practice management system pends this invoice and waits for the final response. Meanwhile the pharmacist is aware that he will be paid, however he doesn't know how much yet.
As the response is being sent to the pharmacy, the payor system forwards the invoice to a Manual Review queue. A claims adjudicator pulls the invoice from the queue and attempts to follow up with the suppliers of the pharmaceutical product to verify the cost being billed. As part of their internal processes, the claims adjudicator will notify the Drug Identification Number Database if the cost of a particular item needs to be modified in the database. In this particular case, this does not occur as the item can be purchased from other suppliers at a lower cost to the pharmacy. However, the claims adjudicator has been able to verify that the cost submitted is correct, is comfortable with the situation and enters the appropriate information into the system authorizing the payment as submitted. The system then generates a final response to the invoice informing the pharmacy that this invoice will be paid in full. Upon receipt of the final response, the pharmacy's practice management system links the invoice to the initial response and the final response, and completes the invoice process.
To demonstrate how a Preferred Accommodation Invoice is created and submitted. An Invoice can represent a single billable line item or multiple billable line items.
This storyboard also depicts delayed adjudication with an initial response. The initial response exchanges Adjudication Manager identifiers and pre-processing information. Full Adjudication Results are created at a later point in time. Delayed infers that the responses will not be immediate and may lag a request by a period of time (perhaps one or more days).
| Inv Request, Init/Comp, PAccom | |
| Inv Init Results Init/Comp, PAccom | |
| Inv Comp Results Init/Comp, PAccom |
Patient Everyman arrives at the hospital for a scheduled admission on Day 1, and requests a Semi-private Room. Upon eligibility check the patient discovers a $200 deductible is owed, and it is paid with a credit card. On Day 2, patient Everyman is transferred to ICU, but is returned to a semi-private room on Day 3. On Day 3 the patient requests a Private Room and is transferred at 9pm. The patient remains in a Private Room until discharge on Day 6.
The hospital submits an Invoice on the discharge day to the insurance company for a 1-night stay in Semi-private ($200) and a 3-night stay in Private ($900), and indicating the paid deductible ($200). A total of $1100 was billed.
The next day (day 7) the insurance company responds with pre-processing results and adjudication related identifiers. It indicates that final adjudication results will follow. Some manual adjudication is required which requires additional time to process the invoice.
On day 8, final adjudication results are received from the insurance company. The full invoiced amount will be paid as requested, less the paid deductible ($200).
To demonstrate how the Invoice Requestor may Nullify an Invoice. An Invoice can include one or more line items for one or more patients. The Nullifylation can apply to all or part of an Invoice. The processing of the Invoice may be in one of the following states when the Nullifylation request is received: pre-adjudication, post adjudication but pre-payment or post payment. If a Payment Advice for the Invoice has already been sent, the Nullifylation request will result in payment adjustments on future Payment Advice statements.
| Inv Nullify Request, Gen | |
| Inv Nullify Results, Comp, Gen |
Mr. Adam Everyman breaks his knee at work. He is taken to the hospital by a co-worker. The doctor at the hospital submits a form stating his injury to HC Payor, Inc. to establish a claim for Adam. The hospital has an established relationship with HC Payor, Inc. and routinely submits Fee for Service claims for payment.
Adam's doctor assesses Adam's injury and recommends him to a (Physiotherapy) treatment plan. The plan is an 8-week therapy program. The program starts next week, one treatment per week. At the end of the program, the doctor will determine whether Adam can return to work.
At the end of the visit, the billing clerk prepares an Invoice and enters the following line items into the Invoice:
-
Ambulance charge
-
Initial Medical treatment charge
The billing clerk of the hospital electronically submits an Invoice to HC Payor, Inc. for adjudication and payment. HC Payor, Inc. immediately responds to the Invoice submission with Adjudication Results, indicating that HC Payor, Inc. has approved all billing line items and will be paid in full by HC Payor, Inc.
At the end of the day, the billing clerk realizes that HC Payor, Inc. should not have been charged the ambulance fee. She submits a cancel request to HC Payor, Inc. to cancel the ambulance charge only. HC Payor, Inc. immediately responds to the Cancel submission with the Cancel Invoice Response, indicating the Invoice number and the payment of the Ambulance charge is cancelled as requested.
Mr. Adam Everyman strains his back at work and goes to see his family physician, Dr. Fay Family. Dr. Family advises him to take a few days off and also determines that Adam will recover much quicker if he buys a massaging chair to relieve the tension and stress off his back. The doctor's office submits a form to HC Payor, Inc. to establish a claim.
Following his doctor's advice, Adam orders a Magnetic Massager from the Level Seven Healthcare, Inc.. The Magnetic Massager costs $700. Adam gives Level Seven Healthcare Inc. his HC Payor Claim Number and requests that the Invoice be submitted directly to HC Payor Inc.. The billing clerk prepares the Invoice and electronically submits it to HC Payor Inc. for adjudication and payment.
HC Payor Inc. responds to the Invoice submission with Adjudication Results, and indicates that HC Payor, Inc. has approved the payment request and $700.00 will be credited to the Level Seven Healthcare, Inc.'s account on the next business day. The salesman tells Adam the massager will be delivered in 30 days.
While waiting for the chair at home, Adam changes his mind and decides to go for a cheaper massaging chair. The Leather Massaging Highback chair only costs $300. He calls Level Seven Healthcare, Inc. and cancels his order for the other chair.
The billing clerk submits a cancel request to HC Payor, Inc. to cancel the Invoice of Magnetic Massager.
HC Payor Inc. immediately responds to the Cancel submission with the Cancel Invoice Response, indicating the Invoice is cancelled as requested and also $700 will be debited from Level Seven Healthcare's account on a subsequent Payment Advice.
To demonstrate how the Invoice Requestor may Nullify an Invoice. An Invoice can include one or more line items for one or more patients. The Nullifylation can apply to all or part of an Invoice. The processing of the Invoice may be in one of the following states when the Nullifylation request is received: pre-adjudication, post adjudication, pre-payment or post payment. If a Payment Advice for the Invoice has already been sent, the Nullifylation request will result in payment adjustments on future Payment Advice statements.
| Inv Nullify Request, Rx | |
| Inv Nullify Results, Comp, Rx |
Ms. Eve Everywoman has diabetes. She goes to the pharmacy with her mother for an insulin refill. When they get there, Eve places her order for a refill and leaves. A few minutes later, the pharmacist starts Eve's order. The pharmacist fills Eve's bottle with Amoxicillin. When she finishes, she electronically sends an Invoice to Eve's insurance company for adjudication and payment. On the Invoice, it indicates that Eve has a bottle of Amoxicillin refill.
HC Payor, Inc, immediately responds to the Invoice submission with Adjudication Results, indicating that it has approved the Invoice and the billing line item will be paid in full.
When Eve returns to take her medication from the pharmacist, she notices that the prescription says she has received a bottle of Amoxicillin and not a bottle of insulin that she ordered. She informs the mistake to the pharmacist.
The pharmacist submits a cancel request to Eve's Insurance Company to cancel the Invoice of the Amoxicillin.
HC Payor, Inc. immediately responds to the Cancel submission with the Cancel Invoice Response, indicating the Invoice is cancelled as requested.
To demonstrate how the Invoice Requestor may Nullify an Invoice. An Invoice can include one or more line items for one or more patients. The Nullifylation can apply to all or part of an Invoice. The processing of the Invoice may be in one of the following states when the Nullifylation request is received: pre-adjudication, post adjudication but pre-payment or post payment. If a Payment Advice for the Invoice has already been sent, the Nullifylation request will result in payment adjustments on future Payment Advice statements.
| Inv Nullify Request, PAccom | |
| Inv Nullify Results, Comp, PAccom |
Patient Everywoman arrives at the hospital for a scheduled admission on Day 1, and requests a Semi-private Room. On Day 2, patient Everywoman is transferred to ICU, but is returned to a semi-private room on Day 3. On Day 3 the patient requests a Private Room and is transferred at 9pm. The patient remains in a Private Room until discharge on Day 6.
The hospital submits an Invoice on the discharge day to the insurance company for a 1-night stay in Semi-private and a 3-night stay in Private. Just as the invoice is sent Patient Everywoman realizes that she recently changed her insurance coverage and that she no longer is covered for private or semi-private accommodation. She informs the hospital and the hospital immediately cancels the invoice to the insurance company. Patient Everywoman pays for the entire accommodation fee with her credit card.
The insurance company responds to the Cancel Request with a Cancel Invoice Response, indicating the Invoice number and the payment of all line items are cancelled as requested. There will be no debit or credit on the Payment Advice since the cancellation occurred prior to adjudication.
To demonstrate the submission of a Generic Invoice Query and the response to the Query. The Query Response will inform the Invoice Requestor of the processing stage of the Invoice and any available Adjudication Results. The closer the Invoice processing is to completion the more information will be provided in the Query Results.
| Inv Query Request, Gen |
Level Seven Healthcare, Inc. and the Home Health Care Clinic has processed and electronically submitted a claim for a special air circulating mattress pad for their patient Mrs.Eve Everywoman. Mrs. Everywoman's family last week had placed an order for this device from the rehab hospital. This was done so it could be installed at her home prior to her hospital discharge.
Mrs. Everywoman has an extended health care policy with HC Payor Inc. HC Payor, Inc. has agreements with certain medical supply vendors for electronic claim submissions and payments. Level Seven healthcare, Inc. is one of their preferred providers.
The electronic claim was submitted last week. Because of the type of device and the dollar amount requested a manual review and assessment from HC Payor, Inc. had to be done before payment would be given. HC Payor Inc. told Home Health Care Clinic, Inc. they would receive a final answer on or before 10 business days and issued them the following claim reference number,
-
9030493295
A few days later Mrs. Everywoman's family stops in to the Home Health Care Clinic to see if payment was received from HC Payor, Inc. Eve was doing so well the hospital was considering an early discharge.
Home Health Care Clinic checks for messages on their system and sees none. An electronic query is submitted to HC Payor Inc. inquiring the status of claim 9030493295. A response from HC Payor Inc. indicates that final claim payment information will be forwarded to them tomorrow.
During a patient's visit to the optometrist, it was determined that the patient would benefit from the use of eyeglasses. The optometrist asked the patient if they had eyeglass coverage with an extended benefit plan. The patient indicated that they did have extended coverage through their employer with HC Payor, Inc,. for $ 500.00 every 2 years.
The patient looked through their wallet and found their HC Payor, Inc. extended benefit coverage card that included the plan ID, group coverage number, insured's ID number, name and DOB and plan expiry date. The receptionist entered this information into their computer system.
The patient selected their eyeglass frames and lenses and the optometrist indicated they would be ready for them to pick up tomorrow afternoon.
Upon completion of the eyeglasses, the receptionist submits an electronic invoice to HC Payor, Inc. for adjudication and payment. After waiting 5 minutes and not receiving an online response, the receptionist submits a query to the insurance company to find out the status of the invoice.
The insurance company immediately responds with a message that the adjudication results for this invoice are not yet available.
The receptionist makes a note to try the query again if she has not received a response from the HC Payor, Inc. in the next 2 hours.
To demonstrate the submission of a Pharmacy Invoice Query and the response to the Query. The Query Response will inform the Invoice Requestor of the processing stage of the Invoice and any available Adjudication Results. The closer the Invoice processing is to completion the more information will be provided in the Query Results.
Good Neighbor Pharmacy is a small volume pharmacy. As a result, the pharmacy is unable to purchase its pharmaceutical items direct from the manufacturer and must rely on a wholesaler. This unfortunately has resulted in the store purchasing some pharmaceutical items at a cost that is greater than what most of the payors will allow. Whenever these items are billed to the payors, they are billed as Cost to Operator invoices.
On January 27, 2002, Good Neighbor Pharmacy processes a Cost to Operator Invoice for a pharmaceutical item that cannot be purchased at the cost that the payor will reimburse. Upon recognizing the Cost to Operator code, the payor system switches the role from Real time to Delayed Initial Response, places the invoice into the Manual Review queue for further investigation, and sends back to the pharmacy the following:
-
The patient is eligible.
-
The drug is eligible.
-
Before final adjudication can occur, manual follow up is required.
-
Final adjudication results will be forwarded within 24 hours.
Upon receipt of this response, the pharmacy's practice management system pends this invoice and waits for the final response. Meanwhile the pharmacist is aware that he will be paid, however he doesn't know how much yet.
After a period of 24 hours, the pharmacy's practice management system notifies the pharmacist that the final adjudication result from the payor for this invoice has not yet been received. The pharmacist, concerned, creates and sends a query asking where in the adjudication process this invoice currently resides. As the claims adjudicator is having difficulty verifying the costing information sent on the original invoice, they have entered a still pending code into the system against this invoice. When the query is received by the payor's system, it recognizes the still pending code and immediately responds with the following message:
-
Manual verification not yet complete
The pharmacist sees this message on his screen, and makes a note to send another query if the final adjudication results have not been sent by the end of the current business day.
To demonstrate the submission of a Preferred Accommodation Invoice Query and the response to the Query. The Query Response will inform the Invoice Requestor of the processing stage of the Invoice and any available Adjudication Results. The closer the Invoice processing is to completion the more information will be provided in the Query Results.
| Inv Query Request, PAccom |
While reconciling the accounts payable, the billing clerk at Good Health Hospital noticed an outstanding invoice previously submitted to HC Payor, Inc. The invoice had been submitted one week earlier for the accommodation charges on the Maternity ward.
The billing clerk submitted a Query Invoice to HC payor, Inc. quoting the Invoice Number.
A query response returned detailing the status of each item on the invoice. 10 of the line items were approved as invoiced, 1 was approved with adjustments, 2 were rejected, and 1 item was marked, Pending Manual Review.
The admission department at Good Health Hospital submitted an invoice to HC Payor, Inc. for recovering the week's preferred accommodation charges. While filing the documentation under Pending Adjudication, the admissions clerk noticed an error on the accommodation charges for Mr. Everyman. The invoice was charging the insurer for 4 night's semi-private accommodation.
Mr. Everyman had spent one night in a semi-private room, but had requested a private room for the remainder of his hospital stay.
The clerk immediately submitted a preferred accommodation query to HC Payor, Inc. to determine the processing status of this one item on the Good Health Invoice.
The response received from HC Payor, Inc, was:
-
Invoice Item Pending Adjudication
The admissions clerk then submitted a Cancel Invoice for Mr. Everyman's accommodation charges, and proceeded to send a new invoice for the correct amount.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of application roles and their relationships in the Version 3 Guide.
An application that is responsible for the submission of Invoices, Chiro Physio for chiro physio sservices provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list of chiro physio services and/or products with expected remuneration (fees). The services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices, Generic for health care services provided and/or products delivered by a generic benefits group on behalf of one or more patients.
An Invoice is an itemized list for services (e.g. diagnosis, treatment) or products (e.g. wheelchair, hearing aid) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices, Hospital for medical services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list of chiro physio services and/or products with expected remuneration (fees). The services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices, Oral Health for oral health services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list of oral health services and/or products with expected remuneration (fees). The services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices, Pharmacy for pharmaceutical services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list for services or products (e.g. prescribed medication, blood glucose meter) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices, Physician for medical services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list of chiro physio services and/or products with expected remuneration (fees). The services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices, Preferred Accommodation for accommodation used by one or more patients.
An Invoice is an itemized list of accommodation with expected remuneration (fees). The accommodation may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices, Vision Care for vision care services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list of vision care services and/or products with expected remuneration (fees). The services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices for health care services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list for services (e.g. diagnosis, treatment) or products (e.g. wheelchair, hearing aid) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices, Chiro Physio for chiro physio services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list for services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive an initial response, which may contain partial results and an indication when the Final Invoice Adjudication Results will be forwarded from the Invoice Manager.
An application that is responsible for the submission of Invoices, Generic for health care services provided and/or products delivered by a generic benefits group on behalf of one or more patients.
An Invoice is an itemized list for services (e.g. diagnosis, treatment) or products (e.g. wheelchair repair, hearing aid) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive an initial response, which may contain partial results and an indication when the Final Invoice Adjudication Results will be forwarded from the Invoice Manager.
An application that is responsible for the submission of Invoices, Oral Health for oral health services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list for services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive an initial response, which may contain partial results and an indication when the Final Invoice Adjudication Results will be forwarded from the Invoice Manager.
An application that is responsible for the submission of Invoices, Pharmacy for pharmaceutical services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list for services or products (e.g. prescribed medication, blood glucose meter) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive an initial response, which may contain partial results and an indication when the Final Invoice Adjudication Results will be forwarded from the Invoice Manager.
An application that is responsible for the submission of Invoices, Physician for medical services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list of chiro physio services and/or products with expected remuneration (fees). The services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices, Preferred Accommodation for accommodation used by one or more patients.
An Invoice is an itemized list of accommodation with expected remuneration (fees). The accommodation may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive an initial response, which may contain partial results and an indication when the Final Invoice Adjudication Results will be forwarded from the Invoice Manager.
An application that is responsible for the submission of Invoices, Vision Care for vision care services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list of chiro physio services and/or products with expected remuneration (fees). The services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive only the Final Invoice Adjudication Results with no initial response from the Invoice Manager.
An application that is responsible for the submission of Invoices for health care services provided and/or products delivered on behalf of one or more patients.
An Invoice is an itemized list for services (e.g. diagnosis, treatment) or products (e.g. wheelchair, hearing aid) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoices that are not fully paid by an Invoice Manager may be submitted to subsequent Invoice Managers (Payors), as long as the Invoice Adjudication Results from the previous Invoice Manager(s) are included in subsequent Invoices. This provides for the handling of Coordination of Benefits (COB).
It is assumed that there is a shared repository of Patient, Invoice, Provider and other "master file" type information between sender and receiver. Therefore messages do not include or expect details on these elements.
The Invoice Requestor will receive an initial response, which may contain partial results and an indication when the Final Invoice Adjudication Results will be forwarded from the Invoice Manager.
An application that responds to an Invoice, Chiro Physio with the Final Invoice Adjudication Results only.
An Invoice is an itemized list for chiro physio services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
The Final Invoice Adjudication Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Invoice by a period of time (perhaps one or more days).
An application that responds to an Invoice, Generic with the Final Invoice Adjudication Results only.
An Invoice is an itemized list for services (e.g. diagnosis, treatment) or products (e.g. wheelchair, hearing aid) delivered by a generic benefits group, with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
The Final Invoice Adjudication Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Invoice by a period of time (perhaps one or more days).
An application that responds to an Invoice, Hospital with the Final Invoice Adjudication Results only.
An Invoice is an itemized list for medical services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
The Final Invoice Adjudication Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Invoice by a period of time (perhaps one or more days).
An application that responds to an Invoice, Oral Health with the Final Invoice Adjudication Results only.
An Invoice is an itemized list for oral health services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
The Final Invoice Adjudication Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Invoice by a period of time (perhaps one or more days).
An application that responds to an Invoice, Pharmacy with the Final Invoice Adjudication Results only.
An Invoice is an itemized list for pharmaceutical services or products (e.g. prescribed medication, blood glucose meter) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
The Final Invoice Adjudication Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Invoice by a period of time (perhaps one or more days).
An application that responds to an Invoice, Physician with the Final Invoice Adjudication Results only.
An Invoice is an itemized list for medical services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
The Final Invoice Adjudication Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Invoice by a period of time (perhaps one or more days).
An application that responds to an Invoice, Preferred Accommodation with the Final Invoice Adjudication Results only.
An Invoice is an itemized list of accommodations with expected remuneration (fees). The accommodation may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
The Final Invoice Adjudication Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Invoice by a period of time (perhaps one or more days).
An application that responds to an Invoice, Vision Care with the Final Invoice Adjudication Results only.
An Invoice is an itemized list for vision care services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
The Final Invoice Adjudication Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Invoice by a period of time (perhaps one or more days).
An application that responds to an Invoice with the Final Invoice Adjudication Results only.
An Invoice is an itemized list for services (e.g. diagnosis, treatment) or products (e.g. wheelchair, hearing aid) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
The Final Invoice Adjudication Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Invoice by a period of time (perhaps one or more days).
An application that responds to an Invoice, Chiro Physio with Final Invoice Adjudication Results if possible. If Final Invoice Adjudication Results are not possible, then the Invoice Manager may respond with Initial Invoice Adjudication Results that can include partial or incomplete processing results and an indication of when the Final Invoice Adjudication Results will be available.
When the Invoice Manager, Initial/Final Results sends the Final Invoice Adjudication Results, they act as an Invoice Notifier. This Application Role includes the Notifier Application Role.
An Invoice is an itemized list for chiro physio services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
An application that responds to an Invoice, Generic with Final Invoice Adjudication Results if possible. If Final Invoice Adjudication Results are not possible, then the Invoice Manager may respond with Initial Invoice Adjudication Results that can include partial or incomplete processing results and an indication of when the Final Invoice Adjudication Results will be available.
When the Invoice Manager, Initial/Final Results sends the Final Invoice Adjudication Results, they act as an Invoice Notifier. This Application Role includes the Notifier Application Role.
An Invoice is an itemized list for services (e.g. diagnosis, treatment) or products (e.g. wheelchair repair, hearing aid) delivered by a generic benefits group with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
An application that responds to an Invoice, Oral Health with Final Invoice Adjudication Results if possible. If Final Invoice Adjudication Results are not possible, then the Invoice Manager may respond with Initial Invoice Adjudication Results that can include partial or incomplete processing results and an indication of when the Final Invoice Adjudication Results will be available.
When the Invoice Manager, Initial/Final Results sends the Final Invoice Adjudication Results, they act as an Invoice Notifier. This Application Role includes the Notifier Application Role.
An Invoice is an itemized list for oral health services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
An application that responds to an Invoice, Pharmacy with Final Invoice Adjudication Results if possible. If Final Invoice Adjudication Results are not possible, then the Invoice Manager may respond with Initial Invoice Adjudication Results that can include partial or incomplete processing results and an indication of when the Final Invoice Adjudication Results will be available.
When the Invoice Manager, Initial/Final Results sends the Final Invoice Adjudication Results, they act as an Invoice Notifier. This Application Role includes the Notifier Application Role.
An Invoice is an itemized list for pharmaceutical services or products (e.g. prescribed medication, blood glucose meter) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
An application that responds to an Invoice, Physician with Final Invoice Adjudication Results if possible. If Final Invoice Adjudication Results are not possible, then the Invoice Manager may respond with Initial Invoice Adjudication Results that can include partial or incomplete processing results and an indication of when the Final Invoice Adjudication Results will be available.
When the Invoice Manager, Initial/Final Results sends the Final Invoice Adjudication Results, they act as an Invoice Notifier. This Application Role includes the Notifier Application Role.
An Invoice is an itemized list for medical services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
An application that responds to an Invoice, Preferred Accomodation with Final Invoice Adjudication Results if possible. If Final Invoice Adjudication Results are not possible, then the Invoice Manager may respond with Initial Invoice Adjudication Results that can include partial or incomplete processing results and an indication of when the Final Invoice Adjudication Results will be available.
When the Invoice Manager, Initial/Final Results sends the Final Invoice Adjudication Results, they act as an Invoice Notifier. This Application Role includes the Notifier Application Role.
An Invoice is an itemized list of accommodations used with expected remuneration (fees). The Accommodation may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
An application that responds to an Invoice, Vision Care with Final Invoice Adjudication Results if possible. If Final Invoice Adjudication Results are not possible, then the Invoice Manager may respond with Initial Invoice Adjudication Results that can include partial or incomplete processing results and an indication of when the Final Invoice Adjudication Results will be available.
When the Invoice Manager, Initial/Final Results sends the Final Invoice Adjudication Results, they act as an Invoice Notifier. This Application Role includes the Notifier Application Role.
An Invoice is an itemized list for vision care services and/or products with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
An application that responds to an Invoice with Final Invoice Adjudication Results if possible. If Final Invoice Adjudication Results are not possible, then the Invoice Manager may respond with Initial Invoice Adjudication Results that can include partial or incomplete processing results and an indication of when the Final Invoice Adjudication Results will be available.
When the Invoice Manager, Initial/Final Results sends the Final Invoice Adjudication Results, they act as an Invoice Notifier. This Application Role includes the Notifier Application Role.
An Invoice is an itemized list for services (e.g. diagnosis, treatment) or products (e.g. wheelchair repair, hearing aid) with expected remuneration (fees). Services and/or products may also include adjustments such as taxes, mark-ups, surcharges or discounts.
Invoice Adjudication Results include paid as submitted, partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
An application responsible for sending notification of Final Invoice Adjudication Results to an Invoice Tracker.
An application responsible for tracking Invoice Adjudication Results from an Invoice Notifier.
An example of an Invoice Tracker could be a head office, accountant or a payee.
|
||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of trigger events in the Version 3 Guide.
| Type: | State-transition based |
| State Transition: | PaymentRequest (FICR_RM600000UV03) |
A trigger to send an Information Invoice Adjudication Request for adjudication of services and/or products for information purposes.
An Invoice is an itemized list of one or more healthcare services or products. The Invoice includes fees for each item for which payment is expected.
Adjudication is the process by which Invoices are evaluated to determine what, if any, payment should be made. Adjudication includes edit checking to ensure appropriate information has been submitted in the required format. Adjudicated results results can either be accepted as submitted, accepted with adjustments or rejected, with reason codes.
| Type: | State-transition based |
| State Transition: | PaymentRequest (FICR_RM600000UV03) |
A trigger to send an Invoice Adjudication Request for adjudication of services and/or products.
An Invoice is an itemized list of one or more healthcare services or products. The Invoice includes fees for each item for which payment is expected.
Adjudication is the process by which Invoices are evaluated to determine what, if any, payment should be made. Adjudication includes edit checking to ensure appropriate information has been submitted in the required format. Adjudicated results results can either be accepted as submitted, accepted with adjustments or rejected, with reason codes.
| Type: | State-transition based |
| State Transition: | PaymentIntent (FICR_RM610000UV03) |
A trigger to send a revised Invoice Adjudication Result, for completed adjudication results that have been previously communicated.
Adjudication is the process by which Invoices are evaluated to determine what, if any, payment should be made. Adjudication includes edit checking to ensure appropriate information has been submitted in the required format.
Adjudication Results for an Invoice include paid as submitted partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
| Type: | Interaction based |
A trigger to send an initial Invoice Adjudication Results when the Adjudicator has completed an initial preprocessing of the Invoice Adjudication Request.
Final results will come later (e.g. next day) as an unsolicited result.
The initial results may include preliminary edits such as patient identifier and date validation as well as patient eligibility validation. The initial results may also indicate when the final results may be expected.
| Type: | State-transition based |
| State Transition: | PaymentIntent (FICR_RM610000UV03) |
A trigger to send a completed Invoice Adjudication Result.
This trigger may be fired close to immediate (i.e., in the same submission/response interaction as the request) or may lag the request by a period of time (perhaps one or more days).
Adjudication is the process by which Invoices are evaluated to determine what, if any, payment should be made. Adjudication includes edit checking to ensure appropriate information has been submitted in the required format.
Adjudication Results for an Invoice include paid as submitted partially paid or refused for each item in the Invoice, with appropriate reason codes explaining why the item was paid or not paid.
| Type: | State-transition based |
| State Transition: | InvoiceElementGroup (FICR_RM660000UV01) |
A trigger to send an Invoice Re-Adjudication Request to the Adjudicator for adjudication of a previously adjudicated Invoice.
In the same manner as the response to an Invoice, the results for an Invoice Re-Adjudication Request are communicated as Invoice Adjudication Results.
| Type: | State-transition based |
| State Transition: | InvoiceElementGroup (FICR_RM630000UV01) |
A trigger that indicated successful completion of an Invoice Nullify Request. In other words, the request has been nullified.
| Type: | State-transition based |
| State Transition: | InvoiceElementGroup (FICR_RM620000UV01) |
A trigger to send an Invoice Nullify Request.
The response to the request may be accepted or rejected, depending on the ability of the Adjudicator to nullify the request.
| Type: | State-transition based |
| State Transition: | InvoiceElementGroup (FICR_RM630000UV01) |
A trigger that indicated unsuccessful completion of an Invoice Nullify Request. In other words, the request has NOT been nullified.
| Type: | User request |
A trigger to send an Iinvoice Query Request to determine the existence and status of an Invoice Adjudication Request.
For example, a pharmacy may realize during their weekly practice management reconciliation that results for an invoice submitted earlier in the week were not received. The pharmacy submits a Invoice Query Request to determine if the invoice has been adjudicated and the processing results of the adjudication.
An Invoice Query Request can be submitted during any stage of Invoice processing: pre-adjudication, post-adjudication. The extent of information provided in the Invoice Query Response will be impacted by the extent to which the Invoice has been processed.
| Type: | Interaction based |
A trigger to send an InvoiceQuery Response indicating the existence and status of an Invoice Adjudication Request.
Invoice Query Response will be impacted by the processing stage of the Invoice: pre-adjudication, post adjudication. The response will inform the Provider of the processing stage of the Invoice and any available adjudication results. The closer the Invoice processing is to completion, the more information will be provided in the response.
|
||||||||||||||||
|
For details on the interpretation of this section, see the description of RMIMs in the Version 3 Guide.
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to submit an Invoice Adjudication Request from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
This request for adjudication and payment is made up of 2 core classes referenced in the RMIM, the FinancialTransaction (cloned as the PaymentRequest) and the InvoiceElement (cloned as the InvoiceElementGroup and InvoiceElementDetail). An invoice message consists of a root InvoiceElementGroup made up of components that are dependent requests for payment and adjudication.
A submitted Invoice is sent to the recipient identified in the message control wrapper and is to be processed by an Adjudicator. The Payor is identified through the Debit act relationship to the A_AccountPayor CMET.
To generate an Invoice (request for payment and adjudication), a PaymentRequest (a FinancialTransaction in RQO: request order mood), InvoiceElementGroup (an InvoiceElement in RQO: request order mood),) and an InvoiceElementDetail (an InvoiceElement in RQO: request order mood),) are created and the acts are related through act relationships and supported by a number of participations (e.g. Covered Party, Provider, Payor, Payee).
The PaymentRequest allows for a grouping of InvoiceElements and reflects the request for payment of a specified monetary amount. The PaymentRequest indicates "Please Pay". The PaymentRequest ties to a root InvoiceElementOrderGroup (to which a set of participations and act relationships are connected to provide information applicable to the whole invoice) that contains one or more InvoiceElementGroups and InvoiceElementDetails sets. See invoice type grouping example diagrams in the Domain Description.
An Authorization may have been obtained for an A InvoiceElementDetail or InvoiceElementGroup that is specified by the InvoiceElementCrossReference.
The InvoiceElement (both group and detail) are the elements of an Invoice that need to be adjudicated in order to determine any payment. There are 2 types of InvoiceElements: a group and a detail. The InvoiceElementDetail identifies the pricing for a line item such as a drug, medical procedure, durable good or other billable item including adjustments (e.g. taxes, discounts, surcharges). The InvoiceElementGroup allows for the grouping/collection of InvoiceElement groups and detail's to make up a logical billable item. For example, a Pharmacy dispense may have a group with 2 details, one for the drug cost and the other for the dispense fee. Both must be present and can be grouped with an InvoiceElementGroup.
Concluding, an Invoice is made up of one PaymentRequest (Please Pay), connected to a root InvoiceElement group, which contains one or more InvoiceElementGroups and InvoiceElementDetails.
Included are the identification data for each of the participants, including Provider's organization, patient(s)/covered party, insured party(policy holder), Payor, Payee and target recipient individuals/organizations. The Payor is the party specified as financially responsible for the Invoice and the Payee the party that will receive any payment. Both of these participations are noted against the PaymentRequest.
Patient(s) are identified as the Covered Party role for the root InvoiceElementGroup. There may be a single patient or an itemized group with individual insurance information.
Insurance information is included in the PolicyOrAccount. Three major roles for an insurance policy are the, CarrierRole, PolicyHolder and CoveredPartyRole. There may be multiple CoveredParties for a single insurance policy, with the CoveredParty role describing why the patient is covered by the insurance policy (e.g. spouse of PolicyHolder). Also, the Accident class identifies the accident type (workplace, motor vehicle, etc. and its location) and date that is the basis for the coverage being referenced. The Observation InjuryCoding in the billable act is to specify the injuries related to the accident.
Specific data about the billable act (what was performed such as treatment procedures, practitioner identification, service location, etc.) are modeled separately and inserted into the appropriate message types created from this model. See the A_Billable CMET for the specific types of billable acts that can be inserted into the generic Invoice structure. Healthcare products and their packaging type and quantity are included through the Product participation against the InvoiceElement group or detail.
The Invoice may optionally reference a contract under which the billing is done (FinancialContract) and attachments (HealthDocumentAttachment) containing any form of supporting information.
When the claimant has multiple insurance coverages (own and through spouse or a child with both parents having coverage, etc.), the invoice is sent in sequence based on insurance rules to each Adjudicator with subsequent Adjudicators receiving the portion of the previous adjudicator(s)'s results that were placed in the A_InvoiceCoordination CMET in the message in the Invoice Adjudication Results. This will explain to the next Payor the outstanding amounts being claimed. Each Adjudicator is sent identical Invoice elements to adjudicate.
| Invoice Adjudication Request Generic | FICR_HD600100UV01 |
| Invoice Adjudication Request Pharmacy | FICR_HD600200UV01 |
| Invoice Adjudication Request Preferred Accommodation | FICR_HD600300UV01 |
| Invoice Adjudication Request Chiro/Physio | FICR_HD600400UV02 |
| Invoice Adjudication Request Oral Health | FICR_HD600500UV03 |
| Invoice Adjudication Request Vision Care | FICR_HD600600UV03 |
| Invoice Adjudication Request Physician | FICR_HD600700UV03 |
| Invoice Adjudication Request Hospital | FICR_HD600800UV03 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to respond to an Invoice Adjudication Request message from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
The Adjudicator uses it to convey the Invoice Adjudication Results.
A submitted Invoice is processed by an Adjudicator and communicated as a PaymentIntent (a FinancialTransaction in INT:intent mood) and one or more AdjudicationResults (an InvoiceElement in EVN:event mood). These are supported by participations for the Payor and Payee.
The Adjudicator responds to an PaymentRequest (Please pay) with a PaymentIntent (I will pay) that includes a set of AdjudicatedInvoiceElementGroups and AdjudicatedInvoiceElementDetails linked to an AdjudicationResult explaining how the Adjudicator has adjudicated each InvoiceElementGroup and InvoiceElementDetail on the Invoice (e.g. pay as submitted, pay as adjusted, reject provide information) and links to the AdjudicationResultsReason and AdjudicationResultsInformation observations to explain and inform about the results returned. A portion of these results is placed in the A_InvoiceCoordination CMET to be passed on to the next adjudicator in coordination of benefits invoicing.
An AdjudicationResults may also reference related adjudication observations such as drug utilization reporting (DUR) information for drug interactions. This is specified using the A_AdjudicationObservation CMET; the CMET allows for multiple types of Adjudicator initiated adjudication observations to be included in an adjudication response to a Provider.
Changes to Payor, Payee and insurance information, if applicable, may also be returned with the adjudication responses.
A reference to a AdjudicationResultRequiredAct to be performed by the provider organization, may also be made. This could be a requirement to print an Explanation of Benefits (EOB) to be supplied to the patient/covered party. Associated with this may be the specification of a print form to be used. This is done by using the FormRole and Form classes.
| Invoice Adjudication Results Generic | FICR_HD610100UV01 |
| Invoice Adjudication Results Pharmacy | FICR_HD610200UV01 |
| Invoice Adjudication Results Preferred Accommodation | FICR_HD610300UV01 |
| Invoice Adjudication Results Chiro/Physio | FICR_HD610400UV02 |
| Invoice Adjudication Results Oral Health | FICR_HD610500UV03 |
| Invoice Adjudication Results Vision Care | FICR_HD610600UV03 |
| Invoice Adjudication Results Physician | FICR_HD610700UV03 |
| Invoice Adjudication Results Hospital | FICR_HD610800UV03 |
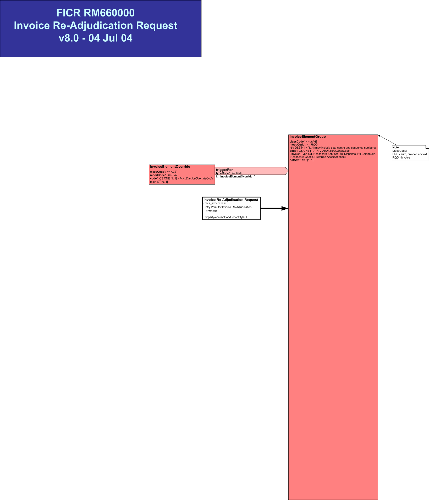
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to submit an Invoice Re-Adjudication message from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
This is a request for another adjudication processing of an existing invoice taking additional or revised information external to the invoice (e.g. billing rate change, adjudication rules changed since original submission) into account.
The class referenced in the model is the InvoiceElement, cloned as the InvoiceElementGroup. This class contains only root group identification and type information to specify which invoice is to be re-processed and the net amount for verification.
The InvoiceElementOverride for the InvoiceElementGroup contains the justification for the re-adjudication.
| Invoice Re-Adjudication Request | FICR_HD660100UV01 |
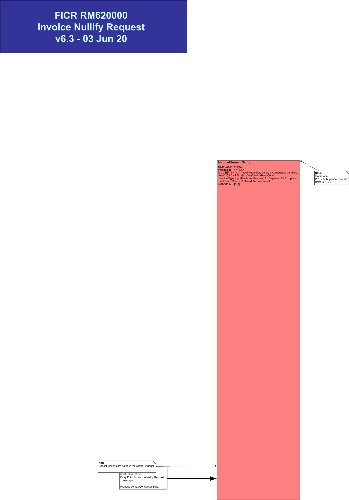
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to submit an Invoice Nullify message from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
This is a request to remove a specified previous request for adjudication and payment of the invoice group referenced. One InvoiceElement, cloned as the root InvoiceElementGroup from the submitted invoice is referenced by identifier without invoicing details. The referenced invoice root group, which contains one or more InvoiceElementGroups and InvoiceElementDetails will be completely nullified. Other data that was included with the referenced invoice is already in the possession of the recipient.
| Invoice Nullify Request | FICR_HD620100UV01 |
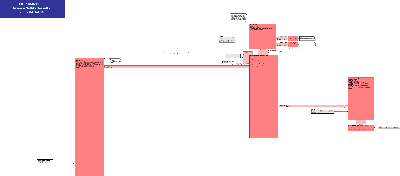
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to respond to an Invoice Nullify Request message from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
This is a response to the request to remove the invoice request for adjudication and payment previously referenced
It is a simple time stamped acknowledgement that is returned if the invoice request had not been processed. If the invoice request for the root group specified has been adjudicated, this message payload will specify the AdjudicatedInvoiceElementGroup with a negative net amount to specify the financial reversal that will be processed.
| Invoice Nullify Results | FICR_HD630100UV01 |
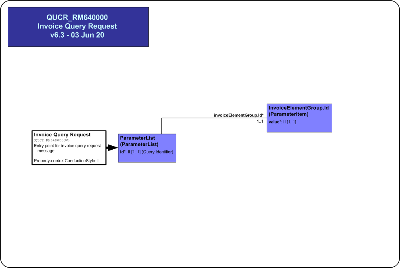
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to send an Invoice Query Request from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
It is used to request the status of Invoice Adjudication Results processing.
A submitted Invoice is processed by an Adjudicator and communicated as an Invoice Adjudication Results message.
When adjudication is completed the Payor responds to a PaymentRequest (Please pay) with a PaymentIntent (I will pay) that includes a set of AdjudicatedInvoiceElement Groups and Details with AdjudicationResults explaining how the Payor has adjudicated each submitted InvoiceElementGroup and InvoiceElementDetail on the Invoice (e.g. pay as submitted, pay as adjusted, reject, provide information). The AdjudicatedInvoiceElement Groups and Details may also indicate a monetary amount if a payment is pending. Changes to Payor, Payee and insurance information, if applicable, may also be returned with the adjudication responses. This information may have previously been sent to the submitter but must be resent in response to a Query Invoice message.
The Invoice Query is a single parameter, the Invoice Element root Group identifier, from the Invoice Request being queried.The Invoice Adjudication Results message is returned in response to this query in the same way it would be returned to the Invoice Adjudication Request message.
This information may have previously been sent to the submitter but must be resent in response to a Invoice Query Request message.
| Invoice Query Request | QUCR_HD640100UV01 |
|
||||||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the description of HMDs in the Version 3 Guide.
This message is a specialization of the Invoice Adjudication Results used to send adjudication results for a Chiro Physio Invoice.
This message is returned to a Provider each time an Invoice Adjudication Request, Chiro Physio message is successfully processed by an Adjudicator Application. As a minimum, the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the invoice and optionally, a tracking number for the Provider Application.
If the Adjudicator Application is able to process the invoice on-line, the Invoice Adjudication Results, Chiro Physio message will contain the Adjudication Results indicating the results of the adjudication (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the invoice will be sent and when adjudication is completed, this message will be sent.
This message is used to send adjudication results for a Generic Invoice.
This message is returned to a Provider each time a Generic Invoice message is successfully processed by a Adjudicator Application. As a minimum, the Invoice Adjudication Results, Generic message will contain the Provider Applications' invoice number, status codes for each Invoice Element Detail Item in the Invoice and optionally, a tracking number for the Adjudicator Application.
If the Adjudicator Application is able to process the invoice on-line, the Invoice Adjudication Results, Generic message will contain the AdjudicationResults indicating the results of the adjudication (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the invoice will be sent and when adjudication is completed, this message will be sent.
This message is a specialization of the Invoice Adjudication Results used to send adjudication results for a Hospital Invoice.
This message is returned to a Provider each time an Invoice Adjudication Request, Physician message is successfully processed by an Adjudicator Application. As a minimum, the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the invoice and optionally, a tracking number for the Provider Application.
If the Adjudicator Application is able to process the invoice on-line, the Invoice Adjudication Results, Physician message will contain the Adjudication Results indicating the results of the adjudication (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the invoice will be sent and when adjudication is completed, this message will be sent.
This message is a specialization of the Invoice Adjudication Results used to send adjudication results for a Oral Health Invoice.
This message is returned to a Provider each time an Invoice Adjudication Request, Oral Health message is successfully processed by an Adjudicator Application. As a minimum, the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the invoice and optionally, a tracking number for the Provider Application.
If the Adjudicator Application is able to process the invoice on-line, the Invoice Adjudication Results, Oral Health message will contain the Adjudication Results indicating the results of the adjudication (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the invoice will be sent and when adjudication is completed, this message will be sent.
This message is a specialization of the Invoice Adjudication Results used to send adjudication results for a Pharmacy Invoice.
This message is returned to a Provider each time an Invoice Adjudication Request, Pharmacy message is successfully processed by an Adjudicator Application. As a minimum, the Invoice Adjudication Results, Pharmacy message will contain the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the invoice and optionally, a tracking number for the Provider Application
If the Adjudicator Application is able to process the invoice on-line, the Invoice Adjudication Results, Pharmacy message will contain the AdjudicationResults indicating the results of the adjudication (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the invoice will be sent and when adjudication is completed, this message will be sent.
This message is a specialization of the Invoice Adjudication Results used to send adjudication results for a Physician Invoice.
This message is returned to a Provider each time an Invoice Adjudication Request, Physician message is successfully processed by an Adjudicator Application. As a minimum, the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the invoice and optionally, a tracking number for the Provider Application.
If the Adjudicator Application is able to process the invoice on-line, the Invoice Adjudication Results, Physician message will contain the Adjudication Results indicating the results of the adjudication (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the invoice will be sent and when adjudication is completed, this message will be sent.
This message is a specialization of the Invoice Adjudication Results used to send adjudication results for a Preferred Accommodation Invoice.
This message is returned to a Provider each time an Invoice Adjudication Request, Preferred Accommodation message is successfully processed by an Adjudicator Application. As a minimum, the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the invoice and optionally, a tracking number for the Provider Application.
If the Adjudicator Application is able to process the invoice on-line, the Invoice Adjudication Results Preferred Accommodation message will contain the AdjudicationResults indicating the results of the adjudication (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the invoice will be sent and when adjudication is completed, this message will be sent.
This message is a specialization of the Invoice Adjudication Results used to send adjudication results for a Vision Care Invoice.
This message is returned to a Provider each time an Invoice Adjudication Request, Vision Care message is successfully processed by an Adjudicator Application. As a minimum, the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the invoice and optionally, a tracking number for the Provider Application.
If the Adjudicator Application is able to process the invoice on-line, the Invoice Adjudication Results, Vision Care message will contain the Adjudication Results indicating the results of the adjudication (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the invoice will be sent and when adjudication is completed, this message will be sent.
This message is used to submit a single Invoice Re-Adjudication Request to a TPA/Payor for processing. The Re-Adjudicate Invoice Request is used by a Provider, to request review of a previously adjudicated Invoice with specification of a Invoice Element root Group within that Invoice. The reason for the Re-Adjudication is provided in the InvoiceElementOverride code and text.
This Re-Adjudication for a Invoice may be requested either because background information, such as a Provider's billing rate may have changed or if some of the adjudication rules have changed since original adjudication of the Invoice.
This message is used to Nullify one Invoice Element root Group that has previously been submitted to an Adjudicator for processing and payment. An Invoice group, and all of its contained group(s) and details, that is Nullified must all be marked as Nullify only and not purged from the Adjudicator Application's database.
The Adjudicator may/may not be able to Nullify the Invoice Element root Group, and will indicate processing results in the response message. In some situations, the invoice has already been paid, and therefore they will hold a debit amount for the Payee until subsequent billing from the Payee utilizes the debit amount.
This message cannot be used to Nullify or remove ancillary information for an Invoice Element group of groups or details such as Authorization or Contact information or any referenced health documents.
This message is used to respond to the Nullify Invoice message that has previously been submitted to an Adjudicator and been processed. The Adjudicator may not have been able to Nullify the Invoice Element root group, and will indicate processing results. In some situations, the Payor has already paid the Invoice Element grouyp, and therefore will hold a debit amount for the Payee until subsequent billing from the Payee utilizes the debit amount.
This message is used by a Provider to request invoice adjudication and invoice processing information.
The Invoice Query is a single parameter, the Invoice Element root Group identifier, from the Invoice Adjudication Request being queried.
The Invoice Adjudication Results message is returned in response to this query in the same way it would be returned to the Invoice Adjudication Request message.
This information may have previously been sent to the submitter but must be resent in response to a Invoice Query Request message.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the definition of Interactions in the Version 3 Guide.
The sender sends an Information Invoice Adjudication Request message for Chiro Physio services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Information Request | FICR_TE600201UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Chiro Physio | FICR_MT600401UV02 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610104UV02 |
| Sender | Invoice Rqstr, Complete Rslts, ChiroPhysio | FICR_AR060004UV02 |
| Receiver | Invoice Mgr, Complete Rslts, ChiroPhysio | FICR_AR062004UV02 |
The sender sends an Information Invoice Adjudication Request message for Generic services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Information Request | FICR_TE600201UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Generic | FICR_MT600101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610101UV01 |
| Sender | Invoice Rqstr, Complete Rslts, Gen | FICR_AR060001UV01 |
| Receiver | Invoice Mgr, Complete Rslts, Gen | FICR_AR062001UV01 |
The sender sends an Information Invoice Adjudication Request message for Pharmacy services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Information Request | FICR_TE600201UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Pharmacy | FICR_MT600201UV01 |
| Sender | Invoice Rqstr, Complete Rslts, Rx | FICR_AR060002UV01 |
| Receiver | Invoice Mgr, Complete Rslts, Rx | FICR_AR062002UV01 |
The sender sends an Information Invoice Adjudication Request message for medical services and/or products rendered by a physician. The sender sends an Information Invoice Adjudication Request message for Physician services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Information Request | FICR_TE600201UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Physician | FICR_MT600701UV03 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610107UV03 |
| Sender | Invoice Rqstr, Complete Rslts, Physician | FICR_AR060007UV03 |
| Receiver | Invoice Mgr, Complete Rslts, Physician | FICR_AR062007UV03 |
The sender sends an Information Invoice Adjudication Request message for Chiro Physio services and/or products.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Information Request | FICR_TE600201UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Chiro Physio | FICR_MT600401UV02 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610204UV02 |
| Initial Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610304UV02 |
| Sender | Invoice Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR061004UV02 |
| Receiver | Invoice Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR063004UV02 |
The sender sends an Information Invoice Adjudication Request message for Generic services and/or products.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Information Request | FICR_TE600201UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Generic | FICR_MT600101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610201UV01 |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610301UV01 |
| Sender | Invoice Rqstr, Init/Comp Rslts, Gen | FICR_AR061001UV01 |
| Receiver | Invoice Mgr, Init/Comp Rslts, Gen | FICR_AR063001UV01 |
The sender sends an Information Invoice Adjudication Request message for Pharmacy services and/or products.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Information Request | FICR_TE600201UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Pharmacy | FICR_MT600201UV01 |
| Reason | Trigger Event | Interaction |
| Initial Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610202UV01 |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610302UV01 |
| Sender | Invoice Rqstr, Init/Comp Rslts, Rx | FICR_AR061002UV01 |
| Receiver | Invoice Mgr, Init/Comp Rslts, Rx | FICR_AR063002UV01 |
The sender sends an Information Invoice Adjudication Request message for medical services and/or products rendered by a physician.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Information Request | FICR_TE600201UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Physician | FICR_MT600701UV03 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610207UV03 |
| Initial Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610307UV03 |
| Sender | Invoice Rqstr, Init/Comp Rslts, Physician | FICR_AR061007UV03 |
| Receiver | Invoice Mgr, Init/Comp Rslts, Physician | FICR_AR063007UV03 |
The sender sends an Invoice Nullify Results message containing the initial results of an Invoice Nullify Request for Chiro Physio services and/or products.
The initial results contain pre-processing information only. The completed results will follow at a later point in time (e.g. next day).
| Trigger Event | Invoice Adjudication Nullify Initial Confirmation | FICR_TE630102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR063004UV02 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR061004UV02 |
The sender sends an Invoice Nullify Results message containing the initial results of an Invoice Nullify Request for Generic services and/or products.
The initial results contain pre-processing information only. The completed results will follow at a later point in time (e.g. next day).
| Trigger Event | Invoice Adjudication Nullify Initial Confirmation | FICR_TE630102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Gen | FICR_AR063001UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Gen | FICR_AR061001UV01 |
The sender sends an Invoice Nullify Results message containing the initial results of an Invoice Nullify Request for Oral Health services and/or products.
The initial results contain pre-processing information only. The completed results will follow at a later point in time (e.g. next day).
| Trigger Event | Invoice Adjudication Nullify Initial Confirmation | FICR_TE630102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, OralHealth | FICR_AR063005UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, OralHealth | FICR_AR061005UV03 |
The sender sends an Invoice Nullify Results message containing the initial results of an Invoice Nullify Request for Pharmacy services and/or products.
The initial results contain pre-processing information only. The completed results will follow at a later point in time (e.g. next day).
| Trigger Event | Invoice Adjudication Nullify Initial Confirmation | FICR_TE630102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Rx | FICR_AR063002UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Rx | FICR_AR061002UV01 |
The sender sends an Invoice Nullify Results message containing the initial results of an Invoice Nullify Request for medical services and/or products rendered by a physician. The sender sends an Invoice Nullify Results message containing the initial results of an Invoice Nullify Request for Physician services and/or products.
The initial results contain pre-processing information only. The completed results will follow at a later point in time (e.g. next day).
The initial results contain pre-processing information only. The completed results will follow at a later point in time (e.g. next day).
| Trigger Event | Invoice Adjudication Nullify Initial Confirmation | FICR_TE630102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Physician | FICR_AR063007UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Physician | FICR_AR061007UV03 |
The sender sends an Invoice Nullify Results message containing the initial results of an Invoice Nullify Request for Preferred Accommodation services and/or products.
The initial results contain pre-processing information only. The completed results will follow at a later point in time (e.g. next day).
| Trigger Event | Invoice Adjudication Nullify Initial Confirmation | FICR_TE630102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, PAccom | FICR_AR063003UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, PAccom | FICR_AR061003UV01 |
The sender sends an Invoice Nullify Results message containing the initial results of an Invoice Nullify Request for Vision Care services and/or products.
The initial results contain pre-processing information only. The completed results will follow at a later point in time (e.g. next day).
| Trigger Event | Invoice Adjudication Nullify Initial Confirmation | FICR_TE630102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, VisionCare | FICR_AR063006UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, VisionCare | FICR_AR061006UV03 |
The sender sends an Invoice Adjudication Results message containing the inital Invoice Adjudication Results for Chiro Physio services and/or products. Completed results will follow at a later point in time (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Chiro Physio | FICR_MT610401UV02 |
| Sender | Invoice Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR063004UV02 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR061004UV02 |
The sender sends an Invoice Adjudication Results message containing the inital Invoice Adjudication Results for Generic services and/or products. Completed results will follow at a later point in time (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Generic | FICR_MT610101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Gen | FICR_AR063001UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Gen | FICR_AR061001UV01 |
The sender sends an Invoice Adjudication Results message containing the inital Invoice Adjudication Results for Oral Health services and/or products. Completed results will follow at a later point in time (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Oral Health | FICR_MT610501UV03 |
| Sender | Invoice Mgr, Init/Comp Rslts, OralHealth | FICR_AR063005UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, OralHealth | FICR_AR061005UV03 |
The sender sends an Invoice Adjudication Results message containing the inital Invoice Adjudication Results for Pharmacy services and/or products. Completed results will follow at a later point in time (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Pharmacy | FICR_MT610201UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Rx | FICR_AR063002UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Rx | FICR_AR061002UV01 |
The sender sends an Invoice Adjudication Results message containing the inital Invoice Adjudication Results for medical services and/or products rendered by a physician. Completed results will follow at a later point in time (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Physician | FICR_MT610701UV03 |
| Sender | Invoice Mgr, Init/Comp Rslts, Physician | FICR_AR063007UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Physician | FICR_AR061007UV03 |
The sender sends an Invoice Adjudication Results message containing the inital Invoice Adjudication Results for Preferred Accommodation services and/or products. Completed results will follow at a later point in time (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Pref Accom | FICR_MT610301UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, PAccom | FICR_AR063003UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, PAccom | FICR_AR061003UV01 |
The sender sends an Invoice Adjudication Results message containing the inital Invoice Adjudication Results for Vision Care services and/or products. Completed results will follow at a later point in time (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Vision Care | FICR_MT610601UV03 |
| Sender | Invoice Mgr, Init/Comp Rslts, VisionCare | FICR_AR063006UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, VisionCare | FICR_AR061006UV03 |
The sender sends an Invoice Adjudication Request message for Chiro Physio services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Chiro Physio | FICR_MT600401UV02 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610104UV02 |
| Sender | Invoice Rqstr, Complete Rslts, ChiroPhysio | FICR_AR060004UV02 |
| Receiver | Invoice Mgr, Complete Rslts, ChiroPhysio | FICR_AR062004UV02 |
The sender sends an Invoice Adjudication Request message for Generic services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Generic | FICR_MT600101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610101UV01 |
| Sender | Invoice Rqstr, Complete Rslts, Gen | FICR_AR060001UV01 |
| Receiver | Invoice Mgr, Complete Rslts, Gen | FICR_AR062001UV01 |
The sender sends an Invoice Adjudication Request message for medical services and/or products rendered by a hospital.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Hospital | FICR_MT600802UV03 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610108UV03 |
| Sender | Invoice Rqstr, Complete Rslts, Hospital | FICR_AR060008UV03 |
| Receiver | Invoice Mgr, Complete Rslts, Hospital | FICR_AR062008UV03 |
The sender sends an Invoice Adjudication Request message for Oral Health services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Oral Health | FICR_MT600501UV03 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610105UV03 |
| Sender | Invoice Rqstr, Complete Rslts, OralHealth | FICR_AR060005UV03 |
| Receiver | Invoice Mgr, Complete Rslts, OralHealth | FICR_AR062005UV03 |
The sender sends an Invoice Adjudication Request message for Pharmacy services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Pharmacy | FICR_MT600201UV01 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610102UV01 |
| Sender | Invoice Rqstr, Complete Rslts, Rx | FICR_AR060002UV01 |
| Receiver | Invoice Mgr, Complete Rslts, Rx | FICR_AR062002UV01 |
The sender sends an Invoice Adjudication Request message for medical services and/or products rendered by a physician.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Physician | FICR_MT600701UV03 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610107UV03 |
| Sender | Invoice Rqstr, Complete Rslts, Physician | FICR_AR060007UV03 |
| Receiver | Invoice Mgr, Complete Rslts, Physician | FICR_AR062007UV03 |
The sender sends an Invoice Adjudication Request message for Preferred Accommodation services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Pref Accom | FICR_MT600301UV01 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610103UV01 |
| Sender | Invoice Rqstr, Complete Rslts, PAccom | FICR_AR060003UV01 |
| Receiver | Invoice Mgr, Complete Rslts, PAccom | FICR_AR062003UV01 |
The sender sends an Invoice Adjudication Request message for Vision Care services and/or products.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Vision Care | FICR_MT600601UV03 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610106UV03 |
| Sender | Invoice Rqstr, Complete Rslts, VisionCare | FICR_AR060006UV03 |
| Receiver | Invoice Mgr, Complete Rslts, Vision Care | FICR_AR062006UV03 |
The sender sends an Invoice Adjudication Request message for Chiro Physio services and/or products.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Chiro Physio | FICR_MT600401UV02 |
| Reason | Trigger Event | Interaction |
| Initial Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610204UV02 |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610304UV02 |
| Sender | Invoice Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR061004UV02 |
| Receiver | Invoice Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR063004UV02 |
The sender sends an Invoice Adjudication Request message for Generic services and/or products.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Generic | FICR_MT600101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610201UV01 |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610301UV01 |
| Sender | Invoice Rqstr, Init/Comp Rslts, Gen | FICR_AR061001UV01 |
| Receiver | Invoice Mgr, Init/Comp Rslts, Gen | FICR_AR063001UV01 |
The sender sends an Invoice Adjudication Request message for Oral Health services and/or products.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Oral Health | FICR_MT600501UV03 |
| Reason | Trigger Event | Interaction |
| Initial Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610205UV03 |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610305UV03 |
| Sender | Invoice Rqstr, Init/Comp Rslts, OralHealth | FICR_AR061005UV03 |
| Receiver | Invoice Mgr, Init/Comp Rslts, OralHealth | FICR_AR063005UV03 |
The sender sends an Invoice Adjudication Request message for Pharmacy services and/or products.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Pharmacy | FICR_MT600201UV01 |
| Reason | Trigger Event | Interaction |
| Initial Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610202UV01 |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610302UV01 |
| Sender | Invoice Rqstr, Init/Comp Rslts, Rx | FICR_AR061002UV01 |
| Receiver | Invoice Mgr, Init/Comp Rslts, Rx | FICR_AR063002UV01 |
The sender sends an Invoice Adjudication Request message for medical services and/or products rendered by a physician
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Physician | FICR_MT600701UV03 |
| Reason | Trigger Event | Interaction |
| Initial Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610207UV03 |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610307UV03 |
| Sender | Invoice Rqstr, Init/Comp Rslts, Physician | FICR_AR061007UV03 |
| Receiver | Invoice Mgr, Init/Comp Rslts, Physician | FICR_AR063007UV03 |
The sender sends an Invoice Adjudication Request message for Preferred Accommodation services and/or products.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Pref Accom | FICR_MT600301UV01 |
| Reason | Trigger Event | Interaction |
| Initial Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610203UV01 |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610303UV01 |
| Sender | Invoice Rqstr, Init/Comp Rslts, PAccom | FICR_AR061003UV01 |
| Receiver | Invoice Mgr, Init/Comp Rslts, PAccom | FICR_AR063003UV01 |
The sender sends an Invoice Adjudication Request message for Vision Care services and/or products.
The receiver will attempt to return completed Invoice Adjudication Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Request | FICR_TE600101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Activate Vision Care | FICR_MT600601UV03 |
| Reason | Trigger Event | Interaction |
| Initial Invoice Adjudication Results | FICR_TE610102UV01 | FICR_IN610206UV03 |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610306UV03 |
| Sender | Invoice Rqstr, Init/Comp Rslts, VisionCare | FICR_AR061006UV03 |
| Receiver | Invoice Mgr, Init/Comp Rslts, VisionCare | FICR_AR063006UV03 |
The sender sends an Invoice Adjudication Results message containing revised completed results of an Invoice Adjudication Request for Chiro Physio services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Revise Notification | FICR_TE610103UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Chiro Physio | FICR_MT610401UV02 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610104UV02 |
| Sender | Invoice Rslts Notifier, ChiroPhysio | FICR_AR064004UV02 |
| Receiver | Invoice Tracker, ChiroPhysio | FICR_AR065004UV02 |
The sender sends an Invoice Adjudication Results message containing revised completed results of an Invoice Adjudication Request for Generic services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Revise Notification | FICR_TE610103UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Generic | FICR_MT610101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610101UV01 |
| Sender | Invoice Rslts Notifier, Gen | FICR_AR064001UV01 |
| Receiver | Invoice Tracker, Gen | FICR_AR065001UV01 |
The sender sends an Invoice Adjudication Results message containing revised completed results of an Invoice Adjudication Request for Oral Health services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Revise Notification | FICR_TE610103UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Oral Health | FICR_MT610501UV03 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610105UV03 |
| Sender | Invoice Rslts Notifier, OralHealth | FICR_AR064005UV03 |
| Receiver | Invoice Tracker, OralHealth | FICR_AR065005UV03 |
The sender sends an Invoice Adjudication Results message containing revised completed results of an Invoice Adjudication Request for Pharmacy services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Revise Notification | FICR_TE610103UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Pharmacy | FICR_MT610201UV01 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610102UV01 |
| Sender | Invoice Rslts Notifier, Rx | FICR_AR064002UV01 |
| Receiver | Invoice Tracker, Rx | FICR_AR065002UV01 |
The sender sends an Invoice Adjudication Results message containing revised completed results of an Invoice Adjudication Request for medical services and/or products rendered by a physician.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Revise Notification | FICR_TE610103UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Physician | FICR_MT610701UV03 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610107UV03 |
| Sender | Invoice Rslts Notifier, Physician | FICR_AR064007UV03 |
| Receiver | Invoice Tracker, Physician | FICR_AR065007UV03 |
The sender sends an Invoice Adjudication Results message containing revised completed results of an Invoice Adjudication Request for Preferred Accommodation services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Revise Notification | FICR_TE610103UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Pref Accom | FICR_MT610301UV01 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610103UV01 |
| Sender | Invoice Rslts Notifier, PAccom | FICR_AR064003UV01 |
| Receiver | Invoice Tracker, PAccom | FICR_AR065003UV01 |
The sender sends an Invoice Adjudication Results message containing revised completed results of an Invoice Adjudication Request for Vision Care services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Revise Notification | FICR_TE610103UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Vision Care | FICR_MT610601UV03 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610106UV03 |
| Sender | Invoice Rslts Notifier, VisionCare | FICR_AR064006UV03 |
| Receiver | Invoice Tracker, VisionCare | FICR_AR065006UV03 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Chiro Physio services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Chiro Physio | FICR_MT610401UV02 |
| Sender | Invoice Mgr, Complete Rslts, ChiroPhysio | FICR_AR062004UV02 |
| Receiver | Invoice Rqstr, Complete Rslts, ChiroPhysio | FICR_AR060004UV02 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Generic services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Generic | FICR_MT610101UV01 |
| Sender | Invoice Mgr, Complete Rslts, Gen | FICR_AR062001UV01 |
| Receiver | Invoice Rqstr, Complete Rslts, Gen | FICR_AR060001UV01 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for medical services and/or products rendered by a hospital.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Hospital | FICR_MT610802UV03 |
| Sender | Invoice Mgr, Complete Rslts, Hospital | FICR_AR062008UV03 |
| Receiver | Invoice Rqstr, Complete Rslts, Hospital | FICR_AR060008UV03 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Oral Health services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Oral Health | FICR_MT610501UV03 |
| Sender | Invoice Mgr, Complete Rslts, OralHealth | FICR_AR062005UV03 |
| Receiver | Invoice Rqstr, Complete Rslts, OralHealth | FICR_AR060005UV03 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Pharmacy services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Pharmacy | FICR_MT610201UV01 |
| Sender | Invoice Mgr, Complete Rslts, Rx | FICR_AR062002UV01 |
| Receiver | Invoice Rqstr, Complete Rslts, Rx | FICR_AR060002UV01 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for medical services and/or products rendered by a physician.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Physician | FICR_MT610701UV03 |
| Sender | Invoice Mgr, Complete Rslts, Physician | FICR_AR062007UV03 |
| Receiver | Invoice Rqstr, Complete Rslts, Physician | FICR_AR060007UV03 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Preferred Accommodation services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Pref Accom | FICR_MT610301UV01 |
| Sender | Invoice Mgr, Complete Rslts, PAccom | FICR_AR062003UV01 |
| Receiver | Invoice Rqstr, Complete Rslts, PAccom | FICR_AR060003UV01 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Vision Care services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Vision Care | FICR_MT610601UV03 |
| Sender | Invoice Mgr, Complete Rslts, Vision Care | FICR_AR062006UV03 |
| Receiver | Invoice Rqstr, Complete Rslts, VisionCare | FICR_AR060006UV03 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Chiro Physio services and/or products.
This notification follows on initial results sent previously.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Chiro Physio | FICR_MT610401UV02 |
| Sender | Invoice Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR063004UV02 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR061004UV02 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Generic services and/or products.
This notification follows on initial results sent previously.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Generic | FICR_MT610101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Gen | FICR_AR063001UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Gen | FICR_AR061001UV01 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Oral Health services and/or products.
This notification follows on initial results sent previously.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Oral Health | FICR_MT610501UV03 |
| Sender | Invoice Mgr, Init/Comp Rslts, OralHealth | FICR_AR063005UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, OralHealth | FICR_AR061005UV03 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Pharmacy services and/or products.
This notification follows on initial results sent previously.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Pharmacy | FICR_MT610201UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Rx | FICR_AR063002UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Rx | FICR_AR061002UV01 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for medical services and/or products rendered by a physician.
This notification follows on initial results sent previously.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Physician | FICR_MT610701UV03 |
| Sender | Invoice Mgr, Init/Comp Rslts, Physician | FICR_AR063007UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Physician | FICR_AR061007UV03 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Preferred Accommodation services and/or products.
This notification follows on initial results sent previously.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Notification | FICR_TE610101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Pref Accom | FICR_MT610301UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, PAccom | FICR_AR063003UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, PAccom | FICR_AR061003UV01 |
The sender sends an Invoice Adjudication Results message containing the completed results of an Invoice Adjudication Request for Vision Care services and/or products.
This notification follows on initial results sent previously.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Adjudication Complete Initial Confirmation | FICR_TE610102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Complete Vision Care | FICR_MT610601UV03 |
| Sender | Invoice Mgr, Init/Comp Rslts, VisionCare | FICR_AR063006UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, VisionCare | FICR_AR061006UV03 |
The sender sends an Invoice Re-Adjudication Request message for Generic services and/or products. The Invoice Re-Adjudication Request may contain a reason and/or text describing conditions that should be considered when the Invoice is re-adjudicated. This may include some additional information pertinent to the Invoice that was not or could not be submitted with the original Invoice.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Re-adjudication Request | FICR_TE660101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Reactivate | FICR_MT660101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610101UV01 |
| Sender | Invoice Rqstr, Complete Rslts, Gen | FICR_AR060001UV01 |
| Receiver | Invoice Mgr, Complete Rslts, Gen | FICR_AR062001UV01 |
The sender sends an Invoice Re-Adjudication Request message for medical services and/or products rendered by a physician. The Invoice Re-Adjudication Request may contain a reason and/or text describing conditions that should be considered when the Invoice is re-adjudicated. This may include some additional information pertinent to the Invoice that was not or could not be submitted with the original Invoice.
The receiver will provide completed Invoice Adjudication Results, NOT initial results.
| Trigger Event | Invoice Re-adjudication Request | FICR_TE660101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Reactivate | FICR_MT660101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Invoice Adjudication Results | FICR_TE610101UV01 | FICR_IN610107UV03 |
| Sender | Invoice Rqstr, Complete Rslts, Physician | FICR_AR060007UV03 |
| Receiver | Invoice Mgr, Complete Rslts, Physician | FICR_AR062007UV03 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Chiro Physio services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Complete Rslts, ChiroPhysio | FICR_AR062004UV02 |
| Receiver | Invoice Rqstr, Complete Rslts, ChiroPhysio | FICR_AR060004UV02 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Generic services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Complete Rslts, Gen | FICR_AR062001UV01 |
| Receiver | Invoice Rqstr, Complete Rslts, Gen | FICR_AR060001UV01 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Oral Health services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Complete Rslts, OralHealth | FICR_AR062005UV03 |
| Receiver | Invoice Rqstr, Complete Rslts, OralHealth | FICR_AR060005UV03 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Pharmacy services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Complete Rslts, Rx | FICR_AR062002UV01 |
| Receiver | Invoice Rqstr, Complete Rslts, Rx | FICR_AR060002UV01 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for medical services and/or products rendered by a physician.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Complete Rslts, Physician | FICR_AR062007UV03 |
| Receiver | Invoice Rqstr, Complete Rslts, Physician | FICR_AR060007UV03 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Preferred Accommodation services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Complete Rslts, PAccom | FICR_AR062003UV01 |
| Receiver | Invoice Rqstr, Complete Rslts, PAccom | FICR_AR060003UV01 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Vision Care services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Complete Rslts, Vision Care | FICR_AR062006UV03 |
| Receiver | Invoice Rqstr, Complete Rslts, VisionCare | FICR_AR060006UV03 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Chiro Physio services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR063004UV02 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR061004UV02 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Generic services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Gen | FICR_AR063001UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Gen | FICR_AR061001UV01 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Oral Health services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, OralHealth | FICR_AR063005UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, OralHealth | FICR_AR061005UV03 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Pharmacy services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Rx | FICR_AR063002UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Rx | FICR_AR061002UV01 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for medical services and/or products rendered by a physician.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, Physician | FICR_AR063007UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, Physician | FICR_AR061007UV03 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Preferred Accommodation services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, PAccom | FICR_AR063003UV01 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, PAccom | FICR_AR061003UV01 |
The sender sends an Invoice Nullify Results message containing the completed results of an Invoice Nullify Request for Vision Care services and/or products.
This message indicates that the Invoice Nullify Request has been successful and the Invoice Adjudication Request has been nullified.
| Trigger Event | Invoice Adjudication Nullify Notification | FICR_TE630101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Response | FICR_MT630101UV01 |
| Sender | Invoice Mgr, Init/Comp Rslts, VisionCare | FICR_AR063006UV03 |
| Receiver | Invoice Rqstr, Init/Comp Rslts, VisionCare | FICR_AR061006UV03 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Chiro Physio services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630104UV02 |
| Sender | Invoice Rqstr, Complete Rslts, ChiroPhysio | FICR_AR060004UV02 |
| Receiver | Invoice Mgr, Complete Rslts, ChiroPhysio | FICR_AR062004UV02 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Generic services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630101UV01 |
| Sender | Invoice Rqstr, Complete Rslts, Gen | FICR_AR060001UV01 |
| Receiver | Invoice Mgr, Complete Rslts, Gen | FICR_AR062001UV01 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Oral Health services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630105UV03 |
| Sender | Invoice Rqstr, Complete Rslts, OralHealth | FICR_AR060005UV03 |
| Receiver | Invoice Mgr, Complete Rslts, OralHealth | FICR_AR062005UV03 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Pharmacy services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630102UV01 |
| Sender | Invoice Rqstr, Complete Rslts, Rx | FICR_AR060002UV01 |
| Receiver | Invoice Mgr, Complete Rslts, Rx | FICR_AR062002UV01 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for medical services and/or products rendered by a physician.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630107UV03 |
| Sender | Invoice Rqstr, Complete Rslts, Physician | FICR_AR060007UV03 |
| Receiver | Invoice Mgr, Complete Rslts, Physician | FICR_AR062007UV03 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Preferred Accommodation services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630103UV01 |
| Sender | Invoice Rqstr, Complete Rslts, PAccom | FICR_AR060003UV01 |
| Receiver | Invoice Mgr, Complete Rslts, PAccom | FICR_AR062003UV01 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Vision Care services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630106UV03 |
| Sender | Invoice Rqstr, Complete Rslts, VisionCare | FICR_AR060006UV03 |
| Receiver | Invoice Mgr, Complete Rslts, Vision Care | FICR_AR062006UV03 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Chiro Physio services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Nullify Invoice Adjudication Results | FICR_TE630102UV01 | FICR_IN630304UV02 |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630404UV02 |
| Sender | Invoice Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR061004UV02 |
| Receiver | Invoice Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR063004UV02 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Generic services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Nullify Invoice Adjudication Results | FICR_TE630102UV01 | FICR_IN630301UV01 |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630401UV01 |
| Sender | Invoice Rqstr, Init/Comp Rslts, Gen | FICR_AR061001UV01 |
| Receiver | Invoice Mgr, Init/Comp Rslts, Gen | FICR_AR063001UV01 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Oral Health services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Nullify Invoice Adjudication Results | FICR_TE630102UV01 | FICR_IN630305UV03 |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630405UV03 |
| Sender | Invoice Rqstr, Init/Comp Rslts, OralHealth | FICR_AR061005UV03 |
| Receiver | Invoice Mgr, Init/Comp Rslts, OralHealth | FICR_AR063005UV03 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Pharmacy services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Nullify Invoice Adjudication Results | FICR_TE630102UV01 | FICR_IN630302UV01 |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630402UV01 |
| Sender | Invoice Rqstr, Init/Comp Rslts, Rx | FICR_AR061002UV01 |
| Receiver | Invoice Mgr, Init/Comp Rslts, Rx | FICR_AR063002UV01 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for medical services and/or products rendered by a physician.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Nullify Invoice Adjudication Results | FICR_TE630102UV01 | FICR_IN630307UV03 |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630407UV03 |
| Sender | Invoice Rqstr, Init/Comp Rslts, Physician | FICR_AR061007UV03 |
| Receiver | Invoice Mgr, Init/Comp Rslts, Physician | FICR_AR063007UV03 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Preferred Accommodation services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Nullify Invoice Adjudication Results | FICR_TE630102UV01 | FICR_IN630303UV01 |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630403UV01 |
| Sender | Invoice Rqstr, Init/Comp Rslts, PAccom | FICR_AR061003UV01 |
| Receiver | Invoice Mgr, Init/Comp Rslts, PAccom | FICR_AR063003UV01 |
The sender sends an Invoice Nullify Request message to request the nullification of a previously submitted Invoice Adjudication Request for Vision Care services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Invoice Adjudication Request.
| Trigger Event | Invoice Adjudication Nullify Request | FICR_TE620101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Invoice Event Nullify Request | FICR_MT620101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Nullify Invoice Adjudication Results | FICR_TE630102UV01 | FICR_IN630306UV03 |
| Completed Nullify Invoice Adjudication Results | FICR_TE630101UV01 | FICR_IN630406UV03 |
| Sender | Invoice Rqstr, Init/Comp Rslts, VisionCare | FICR_AR061006UV03 |
| Receiver | Invoice Mgr, Init/Comp Rslts, VisionCare | FICR_AR063006UV03 |
The sender sends an Invoice Query message to determine the status of a previously submitted Invoice Adjudication Request for Chiro Physio services and/or products.
Query response uses the Invoice Adjudication Results message.
| Trigger Event | Invoice Query Request | QUCR_TE640101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Invoice Event Query Request | QUCR_MT640101UV01 |
| Reason | Trigger Event | Interaction |
| Invoice Query Response | QUCR_TE650101UV01 | QUCR_IN650104UV02 |
| Sender | Invoice Rqstr, Complete Rslts, ChiroPhysio | FICR_AR060004UV02 |
| Receiver | Invoice Mgr, Complete Rslts, ChiroPhysio | FICR_AR062004UV02 |
The sender sends an Invoice Query message to determine the status of a previously submitted Invoice Adjudication Request for Generic services and/or products.
Query response uses the Invoice Adjudication Results message.
| Trigger Event | Invoice Query Request | QUCR_TE640101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Invoice Event Query Request | QUCR_MT640101UV01 |
| Reason | Trigger Event | Interaction |
| Invoice Query Response | QUCR_TE650101UV01 | QUCR_IN650101UV01 |
| Sender | Invoice Rqstr, Complete Rslts, Gen | FICR_AR060001UV01 |
| Receiver | Invoice Mgr, Complete Rslts, Gen | FICR_AR062001UV01 |
The sender sends an Invoice Query message to determine the status of a previously submitted Invoice Adjudication Request for medical services and/or products rendered by a physician.
Query response uses the Invoice Adjudication Results message
| Trigger Event | Invoice Query Request | QUCR_TE640101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Invoice Event Query Request | QUCR_MT640101UV01 |
| Reason | Trigger Event | Interaction |
| Invoice Query Response | QUCR_TE650101UV01 | QUCR_IN650107UV01 |
| Sender | Invoice Rqstr, Complete Rslts, Physician | FICR_AR060007UV03 |
| Receiver | Invoice Mgr, Complete Rslts, Physician | FICR_AR062007UV03 |
The sender sends an Invoice Query message to determine the status of a previously submitted Invoice Adjudication Request for Preferred Accommodation services and/or products.
Query response uses the Invoice Adjudication Results message.
| Trigger Event | Invoice Query Request | QUCR_TE640101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Invoice Event Query Request | QUCR_MT640101UV01 |
| Reason | Trigger Event | Interaction |
| Invoice Query Response | QUCR_TE650101UV01 | QUCR_IN650103UV01 |
| Sender | Invoice Rqstr, Complete Rslts, PAccom | FICR_AR060003UV01 |
| Receiver | Invoice Mgr, Complete Rslts, PAccom | FICR_AR062003UV01 |
The sender sends an Invoice Adjudication Results message containing the processing status (e.g. active, complete) and/or results of an Invoice Adjudication Request for Chiro Physio services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Query Response | QUCR_TE650101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Invoice Event Complete Chiro Physio | FICR_MT610401UV02 |
| Sender | Invoice Mgr, Complete Rslts, ChiroPhysio | FICR_AR062004UV02 |
| Receiver | Invoice Rqstr, Complete Rslts, ChiroPhysio | FICR_AR060004UV02 |
The sender sends an Invoice Adjudication Results message containing the processing status (e.g. active, complete) and/or results of an Invoice Adjudication Request for Generic services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Query Response | QUCR_TE650101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Invoice Event Complete Generic | FICR_MT610101UV01 |
| Sender | Invoice Mgr, Complete Rslts, Gen | FICR_AR062001UV01 |
| Receiver | Invoice Rqstr, Complete Rslts, Gen | FICR_AR060001UV01 |
The sender sends an Invoice Adjudication Results message containing the processing status (e.g. active, complete) and/or results of an Invoice Adjudication Request for Pharmacy services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Query Response | QUCR_TE650101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Invoice Event Complete Pharmacy | FICR_MT610201UV01 |
| Sender | Invoice Mgr, Complete Rslts, Rx | FICR_AR062002UV01 |
| Receiver | Invoice Rqstr, Complete Rslts, Rx | FICR_AR060002UV01 |
The sender sends an Invoice Adjudication Results message containing the processing status (e.g. active, complete) and/or results of an Invoice Adjudication Request for services and / or products rendered by a physician
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Query Response | QUCR_TE650101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Invoice Event Complete Physician | FICR_MT610701UV03 |
| Sender | Invoice Mgr, Complete Rslts, Physician | FICR_AR062007UV03 |
| Receiver | Invoice Rqstr, Complete Rslts, Physician | FICR_AR060007UV03 |
The sender sends an Invoice Adjudication Results message containing the processing status (e.g. active, complete) and/or results of an Invoice Adjudication Request for Preferred Accommodation services and/or products.
Invoice Adjudication Results indicate adjudication results for specified services and/or products, that may generate a payment.
| Trigger Event | Invoice Query Response | QUCR_TE650101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Invoice Event Complete Pref Accom | FICR_MT610301UV01 |
| Sender | Invoice Mgr, Complete Rslts, PAccom | FICR_AR062003UV01 |
| Receiver | Invoice Rqstr, Complete Rslts, PAccom | FICR_AR060003UV01 |
| Return to top of page |

