 ANSI/HL7 V3 CR, R4-2008 HL7 Version 3 Standard: Claims and Reimbursement, Release 4 02/20/2008 |
Content Last Edited: 2009-09-04T22:38:52
5.2 Storyboards
5.3 Application Roles
5.4 Trigger Events
5.5 Refined Message Information Models
5.6 Hierarchical Message Descriptions
5.7 Interactions
Pre-determination provides a mechanism for a Provider to submit a "mock" Invoice and ask the question "If I submitted this item as an Invoice, what would you pay?".
The pre-determination can also be used to submit multiple services and/or products that are similar, in order to determine what the Adjudicator would pay (e.g. name brand drug and generic equivalent). These could be presented to the patient as options in treatment.
The distinction between a pre-determination and an Invoice is that the pre-determination does not result in a payment from the Adjudicator.
The pre-determination also does not imply that the exact same service and/or product, submitted as an Invoice, will be paid as per the pre-determination results. The pre-determination results and Invoice adjudication results can be different for the same service and/or product if there have been intervening Invoices processed against the insurance policy.
A pre-determination number may also be supplied with the pre-determination results and may be required for inclusion in an Invoice
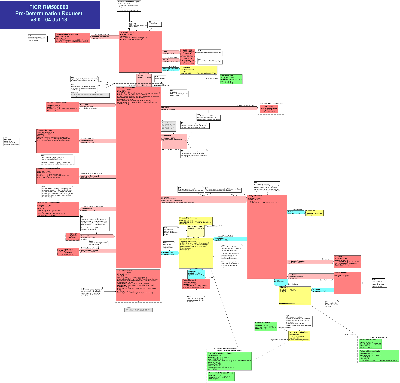
State Transition Diagram
|
||||||||||||
|
For details on the interpretation of this section, see the storyboard discussion in the Version 3 Guide.
To demonstrate how a Chiro Physio Pre-Determination is submitted and adjudicated when there are multiple insurers involved. A Pre-Determination identifies the products and/or services that may be provided in the future. The purpose of submitting a Pre-Determination with COB is to determine whether and how much of the costs will be covered by each insurer.
In situations where Mary Sweep requests Chiropractic services, they are partially covered by the public insurer (provincial) and the residual is covered by her private health insurer (EHC). A Pre-Determination message is sent to the public insurer, the result is sent to the private health insurer in another Pre-Determination message (which includes the public insurer's Pre-Determination result), to determine how much is remaining which will be payable by Mary.
John Driver is involved in a car accident (MVA). His coverage for the related injuries received involves three payors, the public payor (provincial), the extended healthcare (EHC) insurer, and his auto insurer as he has be assessed full blame. John makes an appointment with Dr. Strong at his clinic. The clinic clerk obtains his insurance coverage information. Before treatment has begun, the clinic clerk sends a Pre-Determination message to the public payer. The result received from the public payor specifies that John has coverage for a treatment and the amount that would be paid for the treatment proposed. This resulting information is sent to the private EHC payer, because the full charge has not been paid, in a second Pre-Determination message. The result specifies that since the public payor will pay the specified amount and there is an outstanding amount, they will pay an amount that they specify. There still is an amount remaining not paid by these two payors, therefore the information received is sent to the auto insurer in a third Pre-Determination message. The auto insurer determines that they would pay a specified portion of the amount remaining given that both the public and private insurers have adjudicated the invoice. The amount they will pay is specified in the Adjudication Result message they sent to the clinic. The clinic clerk sees that there is still a portion of the invoice not paid and informs John, when he arrives for the appointment. that the residual will be directly payable by him.
To demonstrate how a Generic Pre-Determination is submitted and adjudicated. A Pre-Determination identifies services that may be rendered in the future. The purpose of submitting a Pre-Determination is to determine whether the services will be covered as well as to identify an estimate for potential payment.
| Pre-Det Request, Gen | |
| Pre-Det Comp Results Comp, Gen |
Mr. Adam Everyman strains his back while at work and goes to see his General Practitioner, Dr. Fay Family, who determines the patient may benefit from physiotherapy. The doctor's office submits a manual form to HC Payor, Inc. to establish a claim. The claim is accepted by the Case Manager, however, Mr. Everyman does not want to go to the physiotherapy clinic that was referred by his health benefit plan for treatment. He would prefer to obtain services from the clinic that a good friend of his works in. Mr. Everyman makes an appointment with the clinic and provides the HC Payor, Inc. claim number and accident date to the receptionist. The receptionist asks for the name of his GP and indicates the first initial visit is covered under his health plan but that if subsequent treatment is required, he would need to determine if HC Payor, Inc. would continue payment.
Seth Stretcher, a practitioner at the clinic and Mr. Everman's friend sees Mr. Everyman for an initial assessment visit. During his assessment, Seth determines that six treatment visits that include back exercise, ultrasound and external massage to the back should be sufficient and should be started immediately. Not knowing whether HC Payor, Inc. will cover the costs of this recommended treatment, Larry asks the receptionist to determine if HC Payor, Inc. will pay for the treatment.
The receptionist prepares a single patient, mult-line item Pre-determination Invoice for on-line submission to HC Payor, Inc. to request payment pre-determination for subsequent treatments. The practice management/billing application in the clinic assigns a unique Invoice number to the Invoice, defaults the Payee for the Invoice, automatically fills in the patient information, patient's insurance coverage, claim number and accident date. The billing clerk enters the 3 therapy procedures that would be provided to the patient:
-
1SJ02YP Exercise therapy, back - using mobility exercise (functional)
-
1SJ07JAAZ Hypothermia, back NEC - using ultrasound device
-
1SJ05JJ Manual therapy, back - using external massage
She also indicates that treatment is required once a week for 6 weeks.
Upon entry and confirmation of the Pre-determination Invoice, the billing clerk submits it to HC Payor, Inc. for payment determination.
HC Payor, Inc. responds immediately to the Pre-determination Invoice submission with Adjudication Results, identifying that if the multi-item invoice is submitted it would likely be paid in full. Note: this is not a commitment to pay by the payor.
To demonstrate how a Pharmacy Pre-Determination is submitted and adjudicated. A Pre-Determination identifies services that may be rendered in the future. The purpose of submitting a Pre-Determination is to determine whether the services will be covered as well as to identify an estimate for potential payment.
| Pre-Det Request, Rx | |
| Pre-Det Comp Results Comp, Rx |
Adam Everyman receives a prescription from his physician, Dr. Fay Family, for Zyban 150 mg to assist him in his attempt to quit smoking. The prescription calls for 60 tablets to be dispensed, with the directions to read "Take one tablet daily for the first three days, then one tablet twice daily thereafter".
Mr. Everyman presents the prescription to his pharmacist, Susan Script, at the Local Pharmacy. Mr. Everyman is a regular patient at the Good Neighbor Pharmacy and his demographic and third party drug plan information is all on file in the pharmacy prescription computer system.
Ms. Script is aware that many drug plans do not include products to assist in smoking cessation as a regular benefit in their drug plan. Ms. Script then enters the pertinent information from the new prescription into the Good Neighbor Pharmacy system and transmits the information as a real time Pre-Determination to Mr. Everyman's third party drug plan adjudicator. The data is processed through the computer system at the third party adjudicator (through the "adjudication engine").
It is determined that Mr. Everyman is eligible to receive benefits, that this drug is a regular benefit under Mr. Everyman's plan and that the quantity of the prescription falls within the drug plan guidelines. The third party adjudicator sends a message to the prescription system at Good neighbor Pharmacy, stating that should a prescription claim be submitted for this product for Mr. Everyman in this quantity, it would likely be paid as a regular benefit. Note that the response is not a commitment from the Payor to pay for this Invoice.
To demonstrate how a Preferred Accommodation Pre-Determination is submitted and adjudicated. A Pre-Determination identifies accommodation that may be provided in the future. The purpose of submitting a Pre-Determination is to determine whether the costs will be covered as well as to identify an estimate for potential payment.
| Pre-Det Request, PAccom | |
| Pre-Det Comp Results Comp, PAccom |
Eve Everywoman is expecting a baby. The due date is in 3 months. Ms. Everywoman would like a private room in the hospital if her insurance company will pay for it. The nightly fee for a private room is $350 and the expected stay for a postpartum mother is three nights. The hospital submits a Pre-determination Invoice to the insurance company for three nights accommodation in a private room at a total cost of $1050.
The insurance company responds immediately with adjudication results indicating that a maximum of two nights private accommodation will be covered for a total of $700 less a $75 co-pay.
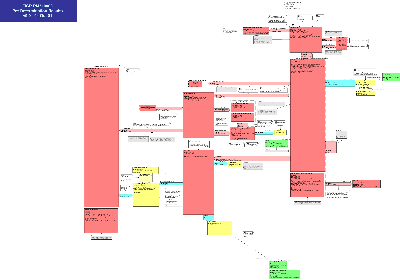
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of application roles and their relationships in the Version 3 Guide.
An application that is responsible for the submission of a Pre-Determination, Chiro Physio for varying services and/or products on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive only the Final Pre-Determination Results with no initial response from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Generic for health care services provided and/or products delivered by a generic benefits group on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive only the Final Pre-Determination Results with no initial response from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Oral Health for varying services and/or products on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive only the Final Pre-Determination Results with no initial response from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Pharmacy for pharmaceutical services provided and/or products delivered on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive only the Final Pre-Determination Results with no initial response from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Physician for varying services and/or products on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive only the Final Pre-Determination Results with no initial response from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Preferred Accommodation for varying types of accommodation on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive only the Final Pre-Determination Results with no initial response from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Vision Care for varying services and/or products on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive only the Final Pre-Determination Results with no initial response from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination for health care services provided and/or products delivered on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive only the Final Pre-Determination Results with no initial response from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Chiro Physio for varying services and/or products on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that is responsible for the submission of a Pre-Determination, Generic for health care services provided and/or products delivered by a generic benefits group on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive an initial response, which may contain partial results and an indication when the Final Pre-Determination Results will be forwarded from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Oral Health for varying services and/or products on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that is responsible for the submission of a Pre-Determination, Pharmacy for pharmaceutical services provided and/or products delivered on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive an initial response, which may contain partial results and an indication when the Final Pre-Determination Results will be forwarded from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Physician for varying services and/or products on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that is responsible for the submission of a Pre-Determination, Preferred Accommodation for varying types of accommodation on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive an initial response, which may contain partial results and an indication when the Final Pre-Determination Results will be forwarded from the Pre-Determination Manager.
An application that is responsible for the submission of a Pre-Determination, Vision Care for varying services and/or products on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that is responsible for the submission of a Pre-Determinations for health care services provided and/or products delivered on behalf of one or more patients.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Pre-Determination Requestor will receive an initial response, which may contain partial results and an indication when the Final Pre-Determination Results will be forwarded from the Pre-Determination Manager.
An application that responds to a Pre-Determination, Chiro Physio with the final Pre-Determination Results only.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Final Pre-Determination Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Pre-Determination Invoice by a period of time (perhaps one or more days).
An application that responds to a Pre-Determination, Generic with the final Pre-Determination Results only.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Final Pre-Determination Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Pre-Determination Invoice by a period of time (perhaps one or more days).
An application that responds to a Pre-Determination, Oral Health with the final Pre-Determination Results only.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Final Pre-Determination Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Pre-Determination Invoice by a period of time (perhaps one or more days).
An application that responds to a Pre-Determination, Pharmacy with the final Pre-Determination Results only.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Final Pre-Determination Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Pre-Determination Invoice by a period of time (perhaps one or more days).
An application that responds to a Pre-Determination, Physician with the final Pre-Determination Results only.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Final Pre-Determination Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Pre-Determination Invoice by a period of time (perhaps one or more days).
An application that responds to a Pre-Determination, Preferred Accommodation with the final Pre-Determination Results only.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Final Pre-Determination Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Pre-Determination Invoice by a period of time (perhaps one or more days).
An application that responds to a Pre-Determination, Vision Care with the final Pre-Determination Results only.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Final Pre-Determination Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Pre-Determination Invoice by a period of time (perhaps one or more days).
An application that responds to a Pre-Determination with the final Pre-Determination Results only.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
The Final Pre-Determination Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Pre-Determination by a period of time (perhaps one or more days).
An application that responds to a Pre-Determination, Chiro Physio with Final Pre-Determination Results if possible. If Final Pre-Determination Results are not possible, then the Pre-Determination Manager may respond with Initial Pre-Determination Results that can include partial or incomplete processing results and an indication of when the Final Pre-Determination Results will be available.
When the Pre-Determination Manager, Initial/Final Results sends the Final Pre-Determination Results, they act as a Pre-Determination Notifier. This Application Role includes the Notifier Application Role.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that responds to a Pre-Determination, Generic with Final Pre-Determination Results if possible. If Final Pre-Determination Results are not possible, then the Pre-Determination Manager may respond with Initial Pre-Determination Results that can include partial or incomplete processing results and an indication of when the Final Pre-Determination Results will be available.
When the Pre-Determination Manager, Initial/Final Results sends the Final Pre-Determination Results, they act as a Pre-Determination Notifier. This Application Role includes the Notifier Application Role.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that responds to a Pre-Determination, Oral Health with Final Pre-Determination Results if possible. If Final Pre-Determination Results are not possible, then the Pre-Determination Manager may respond with Initial Pre-Determination Results that can include partial or incomplete processing results and an indication of when the Final Pre-Determination Results will be available.
When the Pre-Determination Manager, Initial/Final Results sends the Final Pre-Determination Results, they act as a Pre-Determination Notifier. This Application Role includes the Notifier Application Role.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that responds to a Pre-Determination, Pharmacy with Final Pre-Determination Results if possible. If Final Pre-Determination Results are not possible, then the Pre-Determination Manager may respond with Initial Pre-Determination Results that can include partial or incomplete processing results and an indication of when the Final Pre-Determination Results will be available.
When the Pre-Determination Manager, Initial/Final Results sends the Final Pre-Determination Results, they act as a Pre-Determination Notifier. This Application Role includes the Notifier Application Role.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that responds to a Pre-Determination, Physician with Final Pre-Determination Results if possible. If Final Pre-Determination Results are not possible, then the Pre-Determination Manager may respond with Initial Pre-Determination Results that can include partial or incomplete processing results and an indication of when the Final Pre-Determination Results will be available.
When the Pre-Determination Manager, Initial/Final Results sends the Final Pre-Determination Results, they act as a Pre-Determination Notifier. This Application Role includes the Notifier Application Role.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that responds to a Pre-Determination, Preferred Accommodation with Final Pre-Determination Results if possible. If Final Pre-Determination Results are not possible, then the Pre-Determination Manager may respond with Initial Pre-Determination Results that can include partial or incomplete processing results and an indication of when the Final Pre-Determination Results will be available.
When the Pre-Determination Manager, Initial/Final Results sends the Final Pre-Determination Results, they act as a Pre-Determination Notifier. This Application Role includes the Notifier Application Role.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that responds to a Pre-Determination, Vision Care with Final Pre-Determination Results if possible. If Final Pre-Determination Results are not possible, then the Pre-Determination Manager may respond with Initial Pre-Determination Results that can include partial or incomplete processing results and an indication of when the Final Pre-Determination Results will be available.
When the Pre-Determination Manager, Initial/Final Results sends the Final Pre-Determination Results, they act as a Pre-Determination Notifier. This Application Role includes the Notifier Application Role.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application that responds to a Pre-Determination with Final Pre-Determination Results if possible. If Final Pre-Determination Results are not possible, then the Pre-Determination Manager may respond with Initial Pre-Determination Results that can include partial or incomplete processing results and an indication of when the Final Pre-Determination Results will be available.
When the Pre-Determination Manager, Initial/Final Results sends the Final Pre-Determination Results, they act as a Pre-Determination Notifier. This Application Role includes the Notifier Application Role.
A Pre-Determination itemizes products and/or services, which may or may not be delivered/performed in the future, in order to determine whether the items will be covered and to identify an estimate for potential payment. The Pre-Determination Manager (adjudicator) processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice. It must be noted that pre-determination results may only be accurate for that specific moment in time.
An application responsible for sending notification of Final Pre-Determination Results to a Pre-Determination Tracker.
An application responsible for sending notification of Final Pre-Determination Results, Chiro Physio to a Pre-Determination Tracker.
An application responsible for sending notification of Final Pre-Determination Results, Generic to a Pre-Determination Tracker.
An application responsible for sending notification of Final Pre-Determination Results, Pharmacy to a Pre-Determination Tracker.
An application responsible for sending notification of Final Pre-Determination Results, Physician to a Pre-Determination Tracker.
An application responsible for sending notification of Final Pre-Determination Results, Preferred Accommodation to a Pre-Determination Tracker.
An application responsible for tracking Pre-Determination Results from a Pre-Determination Notifier.
An example of a Pre-Determination Tracker could be a head office, accountant or a payee.
An application responsible for tracking Pre-Determination Results, Chiro Physio from a Pre-Determination Notifier.
An example of a Pre-Determination Tracker could be a head office, accountant or a payee.
An application responsible for tracking Pre-Determination Results, Generic from a Pre-Determination Notifier.
An example of a Pre-Determination Tracker could be a head office, accountant or a payee.
An application responsible for tracking Pre-Determination Results, Pharmacy from a Pre-Determination Notifier.
An example of a Pre-Determination Tracker could be a head office, accountant or a payee.
An application responsible for tracking Pre-Determination Results, Preferred Accommodation from a Pre-Determination Notifier.
An example of a Pre-Determination Tracker could be a head office, accountant or a payee.
An application responsible for tracking Pre-Determination Results, Physician from a Pre-Determination Notifier.
An example of a Pre-Determination Tracker could be a head office, accountant or a payee.
|
||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of trigger events in the Version 3 Guide.
| Type: |
A trigger to send a Pre-Determination-Authorization Request for adjudication of services and/or products.
A Pre-Determination-Authorization itemizes services and/or products, which may be rendered in the future, in order to determine whether the items will be covered as well as to identify an estimate for potential payment. The Adjudicator processes the Pre-Determination-Authorization as if it were a real Invoice.
A Provider may also use a Pre-Determination-Authorization Request to compare alternate treatments to determine the least cost alternative for the patient.
| Type: |
A trigger to send a completed Pre-Determination-Authorization Result.
This trigger may be fired close to immediate (i.e., in the same submission/response interaction as the request) or may lag the request by a period of time (perhaps one or more days).
A Pre-Determination-Authorization identifies services and/or products that may be rendered in the future. The purpose of submitting a Pre-Determination-Authorization is to determine whether the Adjudicator will cover the services and/or products as well as to identify an estimate for potential payment.
These results are not an intent to pay; they are informational only. The results indicate items, which would be paid in full, partially paid or refused, with appropriate reason codes explaining why the item would or would not be paid.
| Type: |
A trigger to send an initial Pre-Determination-Authorization Result when the Adjudicator has completed an initial preprocessing of the Pre-Determination-Authorization Request.
Final results will come later (e.g. next day) as an unsolicited result.
The initial results may include preliminary edits such as patient identifier and date validation as well as patient eligibility validation. The initial results may also indicate when the final results may be expected.
| Type: | State-transition based |
| State Transition: | PaymentRequest (FICR_RM500000UV03) |
A trigger to send a Pre-Determination Request for adjudication of services and/or products.
A Pre-Determination itemizes services and/or products, which may be rendered in the future, in order to determine whether the items will be covered as well as to identify an estimate for potential payment. The Adjudicator processes the Pre-Determination as if it were a real Invoice. The only difference between a Pre-Determination and a regular Invoice is that the final result (e.g. payment in full, partial pay) will not result in an actual payment. The Pre-Determination is a mock Invoice.
A Provider may also use a Pre-Determination Request to compare alternate treatments to determine the least cost alternative for the patient.
| Type: | Interaction based |
A trigger to send an initial Pre-Determination Results when the Adjudicator has completed an initial preprocessing of the Pre-Determination Request.
Final results will come later (e.g. next day) as an unsolicited result.
The initial results may include preliminary edits such as patient identifier and date validation as well as patient eligibility validation. The initial results may also indicate when the final results may be expected.
| Type: | State-transition based |
| State Transition: | PaymentIntent (FICR_RM510000UV03) |
A trigger to send a completed Pre-Determination Result.
This trigger may be fired close to immediate (i.e., in the same submission/response interaction as the request) or may lag the request by a period of time (perhaps one or more days).
A Pre-Determination identifies services and/or products that may be rendered in the future. The purpose of submitting a Pre-Determination is to determine whether the Adjudicator will cover the services and/or products as well as to identify an estimate for potential payment.
These results are not an intent to pay; they are informational only. The results indicate items, which would be paid in full, partially paid or refused, with appropriate reason codes explaining why the item would or would not be paid.
| Type: |
A trigger that indicated that the Adjudicator has accepted responsibility for the Pre-Determination Nullify Request and will respond with completed results (accept, reject) at a later point (e.g. next day).
| Type: |
A trigger that indicated successful completion of a Pre-Determination Nullify Request. In other words, the request has been nullified.
| Type: | State-transition based |
| State Transition: | InvoiceElementGroup (FICR_RM520000UV01) |
A trigger to send a Pre-Determination Nullify Request.
The response to the request may be accepted or rejected, depending on the ability of the Adjudicator to nullify the request.
| Type: |
A trigger that indicated unsuccessful completion of a Pre-Determination Nullify Request. In other words, the request has NOT been nullified.
| Type: | User request |
A trigger to send a Pre-Determination Query Request to determine the existence and status of a Pre-Determination Request.
For example, a chiropractor may wish to render a service similar to one submitted on a Pre-Determination the previous day. A Pre-Determination Query Request can be submitted to determine if the service item has been adjudicated and the processing results of the adjudication.
A Pre-Determination Query Request can be submitted during any stage of Pre-Determination processing: pre-adjudication, post-adjudication. The extent of information provided in the Pre-Determination Query Response will be impacted by the extent to which the Pre-Determination has been processed.
| Type: | Interaction based |
A trigger to send a Pre-Determination Query Response indicating the existence and status of a Pre-Determination Request.
Pre-Determination Query Response will be impacted by the processing stage of the Pre-Determination: pre-adjudication, post adjudication. The response will inform the Provider of the processing stage of the Pre-Determination and any available adjudication results. The closer the Pre-Determination processing is to completion, the more information will be provided in the response.
|
||||||||||||
|
For details on the interpretation of this section, see the description of RMIMs in the Version 3 Guide.
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to submit a Pre-Determination Request message from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
The request is for the adjudication of possible future services (or supply of goods) to determine whether they would be covered and to obtain an estimate for the potential payment amount.
The 2 core classes referenced in the RMIM are the FinancialTransaction, cloned as the FinancialTransactionOrderPaymentRequest and the InvoiceElement, cloned as the InvoiceElementOrderGroup and InvoiceElementOrderDetail. As in an invoice, the Pre-Determination Request message can be made up of components that are independent requests for payment and adjudication.
A Pre-Determination Request is sent to the recipient identified in the message control wrapper, an Adjudicator. The Payor is identified through the DebitPayor to the A_Account CMET It is communicated as an FinancialTransactionIntentPayment (a FinancialTransaction in INT:intent mood) and an EventAdjudicationResults (an InvoiceElement in EVN:event mood).
To generate an Invoice (request for payment and adjudication), a FinancialTransactionOrderPaymentRequest (a FinancialTransaction in ORD:order mood), InvoiceElementOrderGroup (an InvoiceElement in ORD:order mood) and an InvoiceElementOrderDetail (an InvoiceElement in ORD:order mood) are created and related through Act Relationships and supported by a number of participations (e.g. patient, Provider, Payor, Payee).
The FinancialTransactionOrderPaymentRequest allows for a grouping of InvoiceElements and reflects the request for payment of a specified monetary amount. The FinancialTransactionOrderPaymentRequest indicates "Please Pay". The leaf level FinancialTransactionOrderPaymentRequest ties to an InvoiceElementOrderGroup; the items below the line (ReasonPaymentRequest) must be adjudicated together. In other words, each ReasonPaymentRequest separates independent billable items.
The InvoiceElement (both group and detail) are the elements of an Invoice that need to be adjudicated in order to determine any payment. There are 2 types of InvoiceElements: a group and a detail. The InvoiceElementOrderDetail identifies the pricing for a line item such as a drug, medical procedure, durable good or other billable item including adjustments (e.g. taxes, discounts, surcharges). The InvoiceElementOrderGroup allows for the grouping/collection of InvoiceElementOrderDetail's to make up a logical billable item. For example, a Pharmacy dispense may have a group with 2 details, one for the drug cost and the other for the dispense fee. Both must be present and can be grouped with an InvoiceElementOrderGroup.
Concluding, an Invoice is made up of one or more FinancialTransactionOrderPaymentRequest (Please Pay), connected to an InvoiceElement grouping, which contains one or more InvoiceElementOrderGroups and InvoiceElementOrderDetails. An Invoice may have multiple FinancialTransactionOrderPaymentRequests, with multiple InvoiceElementOrderGroups and InvoiceElementOrderDetails.
An Authorization may have been obtained for an InvoiceElementOrderDetail or InvoiceElementOrderGroup that is specified by the ConfirmationEventCoverage.
Included are the identification data for each of the participants, including Providers organization, practitioner organization, patient(s), insured party, Payor, Payee, Invoice author and target recipient individuals/organizations. The Payor is the party specified as financially responsible for the Invoice and the Payee the party that will receive any payment. Both of these participations are noted against the FinancialTransactionOrderPaymentRequest.
Patient(s) are identified as the Patient role for the InvoiceElementOrderGroup. There may be a single patient or an itemized group with individual insurance information.
Insurance information is included in the CoverageEventPolicyOrAccount and CoverageDefinition acts. Two major roles for an insurance policy are the PolicyHolder and CoveredPartyRole. There may be multiple CoveredPartys for a single insurance policy, with the CoveredParty role describing why the patient is covered by the insurance policy (e.g. spouse of PolicyHolder). Also, the IncidentEvent, LocationIncident and the R_LocationServiceDelivery CMET classes identify the accident (workplace, motor vehicle, etc. and its location) that is the basis for the coverage being referenced. The ObservationEventInjuryCoding is to specify the injuries related to the accident.
Specific data about the billable act (what was performed such as treatment procedures, practitioner identification, service location, etc.) are modeled separately and inserted into the appropriate message types created from this model. See the A_Billable CMET for the specific types of billable acts that can be inserted into the generic Invoice structure. Healthcare products and their packaging type and quantity are included through the Product participation against the InvoiceElementOrderDetail.
The Invoice may optionally reference a contract under which the billing is done (FinancialContractEvent), accident information (IncidentEvent, including incident type, location and nature of injuries) and attachments (ObservationEventAttachment) containing any form of supporting information.
When the claimant has multiple insurance coverages (own and through spouse or a child with both parents having coverage, etc.), the Invoice is sent in priority sequence based on insurance rules to each Payor with subsequent Payors receiving the Adjudication Results from the previous Payors. Each Payor is sent identical Invoice elements to adjudicate.
Multiple insurance coverages may be prioritized for coordination of benefits submissions. The EventAdjudicationResults from each Payor are forwarded to the next Payor to explain the outstanding amounts being claimed.
| Pre-Determination Request Generic | FICR_HD500100UV01 |
| Pre-Determination Request Pharmacy | FICR_HD500200UV01 |
| Pre-Determination Request Preferred Accommodation | FICR_HD500300UV01 |
| Pre-Determination Request Chiro/Physio | FICR_HD500400UV02 |
| Pre-Determination Request Oral Health | FICR_HD500500UV03 |
| Pre-Determination Request Vision Care | FICR_HD500600UV03 |
| Pre-Determination Request Physician | FICR_HD500700UV03 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents the message used to respond to a Pre-Determination Request from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
A Pre-Determination results is communicated as a PaymentIntent (a FinancialTransaction in INT:intent mood) and one or more AdjudicationResults (an InvoiceElement in EVN:event mood). These are supported by participations for the Payor and Payee.
The Adjudicator responds to a FinancialTransactionOrderPaymentRequest (What might you Pay?) with an FinancialTransactionIntentPayment (I estimate that I would pay) that includes a set of EventAdjudicationResults explaining how each InvoiceElementOrderGroup and InvoiceElementOrderDetail on the Pre-Determination has been adjudicated indicating what they would cover (e.g. pay as submitted, pay as adjusted, reject, provide information). The EventAdjudicationResults may also indicate an estimated monetary amount if the item(s) were covered. Changes to Payor, Payee and insurance information, if applicable, may also be returned with the adjudication responses.
An EventAdjudicationResults may also reference related adjudication observations such as drug utilization reporting (DUR) information for drug interactions. This is specified using the A_AdjudicationObservation CMET; the CMET allows for multiple types of Adjudicator initiated adjudication observations to be included in an adjudication response to a Provider.
A reference to a ActOrderRequired to be performed by the provider organization, may also be made. This could be a requirement to print an Explanation of Benefits (EOB) to be supplied to the patient/covered party. Associated with this may be the specification of a print form to be used. This is done by using the RoleEOBPrintForm and ManufacturedMaterialForm classes.
| Pre-Determination Results Generic | FICR_HD510100UV01 |
| Pre-Determination Results Pharmacy | FICR_HD510200UV01 |
| Pre-Determination Results Preferred Accommodation | FICR_HD510300UV01 |
| Pre-Determination Results Chiro/Physio | FICR_HD510400UV01 |
| Pre-Determination Results Oral Health | FICR_HD510500UV03 |
| Pre-Determination Results Vision Care | FICR_HD510600UV03 |
| Pre-Determination Results Physician | FICR_HD510700UV03 |
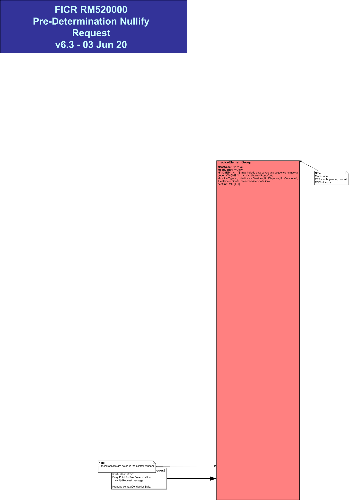
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to submit a Pre-Determination Nullify message from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
This message is a request to remove a specified previous request for Pre-Determination adjudication
The referenced Pre-Determination message was made up of one or more FinancialTransactionOrderPaymentRequests (What might you Pay?), connected to an InvoiceElement root grouping, which contains with one or more InvoiceElementOrderGroups and InvoiceElementOrderDetails. Each one of these root groups must be referenced in a separate nullify message. Only the identification data for the Providers organization, practitioner organization, Payor (the party specified as financially responsible for the Invoice) and the Payee (the party that will receive any payment) are required.
Other data that was included with the referenced Pre-Determination message is already in the possession of the recipient.
| Pre-Determination Nullify Request | FICR_HD520100UV01 |
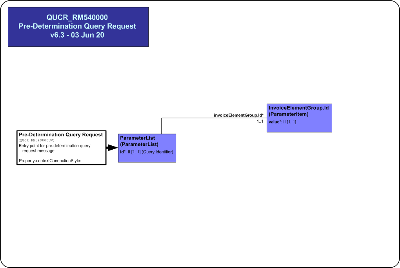
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to send a Pre-Determination Query Request message from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
It is used to request the status of a specific Pre-Determination Request.
A submitted Pre-Determination Request message is processed by an Adjudicator and the response communicated as an Invoice Adjudication Results message.
The Pre-Determination Query is a single parameter, the Invoice Element root Group identifier, from the Pre-Determination Request being queried.
| Pre-Determination Query Request | QUCR_HD540100UV01 |
|
||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the description of HMDs in the Version 3 Guide.
This message is a generic health care products/services Pre-Determination that includes one or more Clincal Product or Clinical Service billable act(s) identifying products/services that may be rendered in the future. The purpose of submitting a Pre-Determination is to determine whether the products/services will be covered as well as to identify an estimate for potential payment.
This message is used to send pre-determination results for a Chiro Physio Pre-Determination.
This message is returned to a Provider each time a Pre-Determination, Chiro Physio message is successfully processed by an Adjudicator Application. As a minimum, the Pre-Determination Results, Chiro Physio message will contain the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the Invoice and optionally, a tracking number for the Adjudicator Application.
If the Adjudicator Application is able to process the Pre-Determination on-line, the Pre-Determination Results Chiro Physio message will contain the A_Adjudication_result indicating the results of the pre-determination (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the Pre-Determination will be sent and when pre-determination is completed, this message will be sent.
This message is used to send pre-determination results for a Generic Pre-Determination.
This message is returned to a Provider each time an Generic Pre-Determination message is successfully processed by an Adjudicator Application. As a minimum, the Pre-Determination Results, Generic message will contain the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the Invoice and optionally, a tracking number for the Adjudicator Application.
If the Adjudicator Application is able to process the Pre-Detemrination on-line, the Pre-Determination Results, Generic message will contain the A_Adjudication_result indicating the results of the pre-determination (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the Pre-Determination will be sent and when adjudication is completed, this message will be sent.
This message is used to send pre-determination results for a Oral Health Pre-Determination.
This message is returned to a Provider each time a Pre-Determination, Oral Health message is successfully processed by an Adjudicator Application. As a minimum, the Pre-Determination Results, Oral Health message will contain the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the Invoice and optionally, a tracking number for the Adjudicator Application.
If the Adjudicator Application is able to process the Pre-Determination on-line, the Pre-Determination Results Oral Health message will contain the A_Adjudication_result indicating the results of the pre-determination (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the Pre-Determination will be sent and when pre-determination is completed, this message will be sent.
This message is used to send pre-determination results for a Pharmacy Pre-Determination.
This message is returned to a Provider each time a Pre-Determination, Pharmacy message is successfully processed by an Adjudicator Application. As a minimum, the Pre-Determination Results, Pharmacy message will contain the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the Invoice and optionally, a tracking number for the Adjudicator Application.
If the Adjudicator Application is able to process the Pre-Determination on-line, the Pre-Determination Results, Pharmacy message will contain the A_Adjudication_result indicating the results of the pre-determination (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the Pre-Determination will be sent and when adjudication is completed, this message will be sent.
This message is used to send pre-determination results for a Physician Pre-Determination.
This message is returned to a Provider each time a Pre-Determination, Physician message is successfully processed by an Adjudicator Application. As a minimum, the Pre-Determination Results, Physician message will contain the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the Invoice and optionally, a tracking number for the Adjudicator Application.
If the Adjudicator Application is able to process the Pre-Determination on-line, the Pre-Determination Results Physician message will contain the A_Adjudication_result indicating the results of the pre-determination (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the Pre-Determination will be sent and when pre-determination is completed, this message will be sent.
This message is used to send pre-determination results for a Preferred Accommodation Pre-Determination.
This message is returned to a Provider each time a Pre-Determination, Preferred Accommodation message is successfully processed by an Adjudicator Application. As a minimum, the Pre-Determination Results, Preferred Accommodation message will contain the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the Invoice and optionally, a tracking number for the Adjudicator Application.
If the Adjudicator Application is able to process the Pre-Determination on-line, the Pre-Determination Results Preferred Accommodation message will contain the A_Adjudication_result indicating the results of the pre-determination (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the Pre-Determination will be sent and when pre-determination is completed, this message will be sent.
This message is used to send pre-determination results for a Vision Care Pre-Determination.
This message is returned to a Provider each time a Pre-Determination, Vision Care message is successfully processed by an Adjudicator Application. As a minimum, the Pre-Determination Results, Vision Care message will contain the Adjudicator Applications' Invoice number, status codes for each Invoice Element Detail Item in the Invoice and optionally, a tracking number for the Adjudicator Application.
If the Adjudicator Application is able to process the Pre-Determination on-line, the Pre-Determination Results Vision Care message will contain the A_Adjudication_result indicating the results of the pre-determination (e.g., paid as submitted, paid as adjusted, etc.). Otherwise an acknowledgement of receipt of the Pre-Determination will be sent and when pre-determination is completed, this message will be sent.
This message is used to Nullify an entire root group of a Pre-Determination that has previously been submitted to a Adjudicator for processing and payment. A Pre-Determination that is Nullified must be marked as Nullified only and not purged from the Adjudicator Application's database.
The Adjudicator may/may not be able to Nullify the Pre-Determination Invoice Element root group, and will indicate processing results in the response message.
This message cannot be used to Nullify or remove ancillary information for a Pre-Determination and/or Invoice Element Detail item such as Contact information or any referenced health documents.
This message is used by a Provider to request previously submitted Pre-Determination invoice processing information.
The Pre-Determination Query is used to query against an entire Pre-Determination Request.
The Pre-Determination Query is a single parameter, the Invoice Element root Group identifier, from the Pre-Determination Request being queried.
The Invoice Adjudication Results message is returned in response to this query in the same way it would be returned to the Pre-Determination Request message.
This information may have previously been sent to the submitter but must be resent in response to a Pre-Determination Query message.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the definition of Interactions in the Version 3 Guide.
The sender sends a Pre-Determination Results message containing the inital Pre-Determination Results for Chiro Physio services and/or products. Completed results will follow at a later point in time (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Initial Confirmation | FICR_TE510102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Chiro Physio | FICR_MT510401UV01 |
| Sender | Pre-Det Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR053004UV02 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR051004UV02 |
The sender sends a Pre-Determination Results message containing the inital Pre-Determination Results for Generic services and/or products. Completed results will follow at a later point in time (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Initial Confirmation | FICR_TE510102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Generic | FICR_MT510101UV01 |
| Sender | Pre-Det Mgr, Init/Comp Rslts, Gen | FICR_AR053001UV01 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, Gen | FICR_AR051001UV01 |
The sender sends a Pre-Determination Results message containing the inital Pre-Determination Results for Oral Health services and/or products. Completed results will follow at a later point in time (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Initial Confirmation | FICR_TE510102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Oral Health | FICR_MT510501UV03 |
| Sender | Pre-Det Mgr, Init/Comp Rslts OralHealth | FICR_AR053005UV03 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, OralHealth | FICR_AR051005UV03 |
The sender sends a Pre-Determination Results message containing the inital Pre-Determination Results for Pharmacy services and/or products. Completed results will follow at a later point in time (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Initial Confirmation | FICR_TE510102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Pharmacy | FICR_MT510201UV01 |
| Sender | Pre-Det Mgr, Init/Comp Rslts, Rx | FICR_AR053002UV01 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, Rx | FICR_AR051002UV01 |
The sender sends a Pre-Determination Results message containing the inital Pre-Determination Results for medical services and/or products rendered by a physician. Completed results will follow at a later point in time (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Initial Confirmation | FICR_TE510102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Physician | FICR_MT510701UV03 |
| Sender | Pre-Det Mgr, Init/Comp Rslts Physician | FICR_AR053007UV03 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, Physician | FICR_AR051007UV03 |
The sender sends a Pre-Determination Results message containing the inital Pre-Determination Results for Preferred Accommodation services and/or products. Completed results will follow at a later point in time (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Initial Confirmation | FICR_TE510102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Pref Accom | FICR_MT510301UV01 |
| Sender | Pre-Det Mgr, Init/Comp Rslts, PAccom | FICR_AR053003UV01 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, PAccom | FICR_AR051003UV01 |
The sender sends a Pre-Determination Results message containing the inital Pre-Determination Results for Vision Care services and/or products. Completed results will follow at a later point in time (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Initial Confirmation | FICR_TE510102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Chiro Physio | FICR_MT500401UV02 |
| Sender | Pre-Det Mgr, Init/Comp Rslts VisionCare | FICR_AR053006UV03 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, VisionCare | FICR_AR051006UV03 |
The sender sends a Pre-Determination Request message for Chiro Physio services and/or products.
The receiver will provide completed Pre-Determination Results, NOT initial results.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Chiro Physio | FICR_MT500401UV02 |
| Reason | Trigger Event | Interaction |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510104UV02 |
| Sender | Pre-Det Rqstr, Comp Rslts, ChiroPhysio | FICR_AR050004UV02 |
| Receiver | Pre-Det Mgr, Comp Rslts, ChiroPhysio | FICR_AR052004UV02 |
The sender sends a Pre-Determination Request message for Generic services and/or products.
The receiver will provide completed Pre-Determination Results, NOT initial results.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Generic | FICR_MT500101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510101UV01 |
| Sender | Pre-Det Rqstr, Complete Rslts, Gen | FICR_AR050001UV01 |
| Receiver | Pre-Det Mgr, Complete Rslts, Gen | FICR_AR052001UV01 |
The sender sends a Pre-Determination Request message for Oral Health services and/or products.
The receiver will provide completed Pre-Determination Results, NOT initial results.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Oral Health | FICR_MT500501UV03 |
| Reason | Trigger Event | Interaction |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510105UV03 |
| Sender | Pre-Det Rqstr, Comp Rslts, OralHealth | FICR_AR050005UV03 |
| Receiver | Pre-Det Mgr, Comp Rslts, OralHealth | FICR_AR052005UV03 |
The sender sends a Pre-Determination Request message for Pharmacy services and/or products.
The receiver will provide completed Pre-Determination Results, NOT initial results.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Pharmacy | FICR_MT500201UV01 |
| Reason | Trigger Event | Interaction |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510102UV01 |
| Sender | Pre-Det Rqstr, Complete Rslts, Rx | FICR_AR050002UV01 |
| Receiver | Pre-Det Mgr, Complete Rslts, Rx | FICR_AR052002UV01 |
The sender sends a Pre-Determination Request message for medical services and/or products rendered by a physician.
The receiver will provide completed Pre-Determination Results, NOT initial results.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Physician | FICR_MT500701UV03 |
| Reason | Trigger Event | Interaction |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510107UV03 |
| Sender | Pre-Det Rqstr, Comp Rslts, Physician | FICR_AR050007UV03 |
| Receiver | Pre-Det Mgr, Comp Rslts, Physician | FICR_AR052007UV03 |
The sender sends a Pre-Determination Request message for Preferred Accommodation services and/or products.
The receiver will provide completed Pre-Determination Results, NOT initial results.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Pref Accom | FICR_MT500301UV01 |
| Reason | Trigger Event | Interaction |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510103UV01 |
| Sender | Pre-Det Rqstr, Comp Rslts, PAccom | FICR_AR050003UV01 |
| Receiver | Pre-Det Mgr, Comp Rslts, PAccom | FICR_AR052003UV01 |
The sender sends a Pre-Determination Request message for Vision Care services and/or products.
The receiver will provide completed Pre-Determination Results, NOT initial results.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Vision Care | FICR_MT500601UV03 |
| Reason | Trigger Event | Interaction |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510106UV03 |
| Sender | Pre-Det Rqstr, Comp Rslts, VisionCare | FICR_AR050006UV03 |
| Receiver | Pre-Det Mgr, Comp Rslts, VisionCare | FICR_AR052006UV03 |
The sender sends a Pre-Determination Request message for Chiro Physio services and/or products.
The receiver will attempt to return completed Pre-Determination Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Chiro Physio | FICR_MT500401UV02 |
| Reason | Trigger Event | Interaction |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510204UV02 |
| Initial Pre-Determination Results | FICR_TE510102UV01 | FICR_IN510304UV02 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR051004UV02 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR053004UV02 |
The sender sends a Pre-Determination Request message for Generic services and/or products.
The receiver will attempt to return completed Pre-Determination Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Generic | FICR_MT500101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Pre-Determination Results | FICR_TE510102UV01 | FICR_IN510201UV01 |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510301UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, Gen | FICR_AR051001UV01 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts, Gen | FICR_AR053001UV01 |
The sender sends a Pre-Determination Request message for Oral Health services and/or products.
The receiver will attempt to return completed Pre-Determination Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Oral Health | FICR_MT500501UV03 |
| Reason | Trigger Event | Interaction |
| Initial Pre-Determination Results | FICR_TE510102UV01 | FICR_IN510205UV03 |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510301UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, OralHealth | FICR_AR051005UV03 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts OralHealth | FICR_AR053005UV03 |
The sender sends a Pre-Determination Request message for Pharmacy services and/or products.
The receiver will attempt to return completed Pre-Determination Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Pharmacy | FICR_MT500201UV01 |
| Reason | Trigger Event | Interaction |
| Initial Pre-Determination Results | FICR_TE510102UV01 | FICR_IN510202UV01 |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510302UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, Rx | FICR_AR051002UV01 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts, Rx | FICR_AR053002UV01 |
The sender sends a Pre-Determination Request message for medical services and/or products rendered by a physician.
The receiver will attempt to return completed Pre-Determination Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Physician | FICR_MT500701UV03 |
| Reason | Trigger Event | Interaction |
| Initial Pre-Determination Results | FICR_TE510102UV01 | FICR_IN510207UV03 |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510307UV03 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, Physician | FICR_AR051007UV03 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts Physician | FICR_AR053007UV03 |
The sender sends a Pre-Determination Request message for Preferred Accommodation services and/or products.
The receiver will attempt to return completed Pre-Determination Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Pref Accom | FICR_MT500301UV01 |
| Reason | Trigger Event | Interaction |
| Initial Pre-Determination Results | FICR_TE510102UV01 | FICR_IN510203UV01 |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510303UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, PAccom | FICR_AR051003UV01 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts, PAccom | FICR_AR053003UV01 |
The sender sends a Pre-Determination Request message for Vision Care services and/or products.
The receiver will attempt to return completed Pre-Determination Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Request | FICR_TE500101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Activate Vision Care | FICR_MT500601UV03 |
| Reason | Trigger Event | Interaction |
| Initial Pre-Determination Results | FICR_TE510102UV01 | FICR_IN510206UV03 |
| Completed Pre-Determination Results | FICR_TE510101UV01 | FICR_IN510306UV03 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, VisionCare | FICR_AR051006UV03 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts VisionCare | FICR_AR053006UV03 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Chiro Physio services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Chiro Physio | FICR_MT510401UV01 |
| Sender | Pre-Det Mgr, Comp Rslts, ChiroPhysio | FICR_AR052004UV02 |
| Receiver | Pre-Det Rqstr, Comp Rslts, ChiroPhysio | FICR_AR050004UV02 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Generic services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Generic | FICR_MT510101UV01 |
| Sender | Pre-Det Mgr, Complete Rslts, Gen | FICR_AR052001UV01 |
| Receiver | Pre-Det Rqstr, Complete Rslts, Gen | FICR_AR050001UV01 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Oral Health services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Oral Health | FICR_MT510501UV03 |
| Sender | Pre-Det Mgr, Comp Rslts, OralHealth | FICR_AR052005UV03 |
| Receiver | Pre-Det Rqstr, Comp Rslts, OralHealth | FICR_AR050005UV03 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Pharmacy services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Pharmacy | FICR_MT510201UV01 |
| Sender | Pre-Det Mgr, Complete Rslts, Rx | FICR_AR052002UV01 |
| Receiver | Pre-Det Rqstr, Complete Rslts, Rx | FICR_AR050002UV01 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for medical services and/or products rendered by a physician.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Physician | FICR_MT510701UV03 |
| Sender | Pre-Det Mgr, Comp Rslts, Physician | FICR_AR052007UV03 |
| Receiver | Pre-Det Rqstr, Comp Rslts, Physician | FICR_AR050007UV03 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Preferred Accommodation services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Pref Accom | FICR_MT510301UV01 |
| Sender | Pre-Det Mgr, Comp Rslts, PAccom | FICR_AR052003UV01 |
| Receiver | Pre-Det Rqstr, Comp Rslts, PAccom | FICR_AR050003UV01 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Vision Care services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Vision Care | FICR_MT510601UV03 |
| Sender | Pre-Det Mgr, Comp Rslts, VisionCare | FICR_AR052006UV03 |
| Receiver | Pre-Det Rqstr, Comp Rslts, VisionCare | FICR_AR050006UV03 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Chiro Physio services and/or products.
This notification follows on initial results sent previously.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Chiro Physio | FICR_MT510401UV01 |
| Sender | Pre-Det Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR053004UV02 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR051004UV02 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Generic services and/or products.
This notification follows on initial results sent previously.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Generic | FICR_MT510101UV01 |
| Sender | Pre-Det Mgr, Init/Comp Rslts, Gen | FICR_AR053001UV01 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, Gen | FICR_AR051001UV01 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Oral Health services and/or products.
This notification follows on initial results sent previously.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Oral Health | FICR_MT510501UV03 |
| Sender | Pre-Det Mgr, Init/Comp Rslts OralHealth | FICR_AR053005UV03 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, OralHealth | FICR_AR051005UV03 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Pharmacy services and/or products.
This notification follows on initial results sent previously.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Pharmacy | FICR_MT510201UV01 |
| Sender | Pre-Det Mgr, Init/Comp Rslts, Rx | FICR_AR053002UV01 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, Rx | FICR_AR051002UV01 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for medical services and/or products rendered by a physician.
This notification follows on initial results sent previously.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Physician | FICR_MT510701UV03 |
| Sender | Pre-Det Mgr, Init/Comp Rslts Physician | FICR_AR053007UV03 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, Physician | FICR_AR051007UV03 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Preferred Accommodation services and/or products.
This notification follows on initial results sent previously.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Pref Accom | FICR_MT510301UV01 |
| Sender | Pre-Det Mgr, Init/Comp Rslts, PAccom | FICR_AR053003UV01 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, PAccom | FICR_AR051003UV01 |
The sender sends a Pre-Determination Results message containing the completed results of a Pre-Determination Request for Vision Care services and/or products.
This notification follows on initial results sent previously.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Complete Notification | FICR_TE510101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Complete Vision Care | FICR_MT510601UV03 |
| Sender | Pre-Det Mgr, Init/Comp Rslts VisionCare | FICR_AR053006UV03 |
| Receiver | Pre-Det Rqstr, Init/Comp Rslts, VisionCare | FICR_AR051006UV03 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Chiro Physio services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Comp Rslts, ChiroPhysio | FICR_AR050004UV02 |
| Receiver | Pre-Det Mgr, Comp Rslts, ChiroPhysio | FICR_AR052004UV02 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Generic services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Complete Rslts, Gen | FICR_AR050001UV01 |
| Receiver | Pre-Det Mgr, Complete Rslts, Gen | FICR_AR052001UV01 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Oral Health services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Comp Rslts, OralHealth | FICR_AR050005UV03 |
| Receiver | Pre-Det Mgr, Comp Rslts, OralHealth | FICR_AR052005UV03 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Pharmacy services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Complete Rslts, Rx | FICR_AR050002UV01 |
| Receiver | Pre-Det Mgr, Complete Rslts, Rx | FICR_AR052002UV01 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for medical services and/or products rendered by a physician.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Comp Rslts, Physician | FICR_AR050007UV03 |
| Receiver | Pre-Det Mgr, Comp Rslts, Physician | FICR_AR052007UV03 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Preferred Accommodation services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Comp Rslts, PAccom | FICR_AR050003UV01 |
| Receiver | Pre-Det Mgr, Comp Rslts, PAccom | FICR_AR052003UV01 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Vision Care services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Comp Rslts, VisionCare | FICR_AR050006UV03 |
| Receiver | Pre-Det Mgr, Comp Rslts, VisionCare | FICR_AR052006UV03 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Chiro Physio services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR051004UV02 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts, ChiroPhysio | FICR_AR053004UV02 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Generic services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, Gen | FICR_AR051001UV01 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts, Gen | FICR_AR053001UV01 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Oral Health services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, OralHealth | FICR_AR051005UV03 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts OralHealth | FICR_AR053005UV03 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Pharmacy services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, Rx | FICR_AR051002UV01 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts, Rx | FICR_AR053002UV01 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for medical services and/or products rendered by a physician.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, Physician | FICR_AR051007UV03 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts Physician | FICR_AR053007UV03 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Preferred Accommodation services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, PAccom | FICR_AR051003UV01 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts, PAccom | FICR_AR053003UV01 |
The sender sends a Pre-Determination Nullify Request message to request the nullification of a previously submitted Pre-Determination Request for Vision Care services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Pre-Determination Request.
| Trigger Event | Pre-Determination Nullify Request | FICR_TE520101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Pre-Determination Event Nullify Request | FICR_MT520101UV01 |
| Sender | Pre-Det Rqstr, Init/Comp Rslts, VisionCare | FICR_AR051006UV03 |
| Receiver | Pre-Det Mgr, Init/Comp Rslts VisionCare | FICR_AR053006UV03 |
The sender sends a Pre-Determination Query message to determine the status of a previously submitted Pre-Determination Request for Chiro Physio services and/or products.
Query response uses the Pre-Determination Results message.
| Trigger Event | Pre-Determination Query Request | QUCR_TE540101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Pre-Determination Event Query Request | QUCR_MT540101UV01 |
| Reason | Trigger Event | Interaction |
| Pre-Determination Query Response | QUCR_TE550101UV01 | QUCR_IN550104UV02 |
| Sender | Pre-Det Rqstr, Comp Rslts, ChiroPhysio | FICR_AR050004UV02 |
| Receiver | Pre-Det Mgr, Comp Rslts, ChiroPhysio | FICR_AR052004UV02 |
The sender sends a Pre-Determination Query message to determine the status of a previously submitted Pre-Determination Request for Generic services and/or products.
Query response uses the Pre-Determination Results message.
| Trigger Event | Pre-Determination Query Request | QUCR_TE540101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Pre-Determination Event Query Request | QUCR_MT540101UV01 |
| Reason | Trigger Event | Interaction |
| Pre-Determination Query Response | QUCR_TE550101UV01 | QUCR_IN550101UV01 |
| Sender | Pre-Det Rqstr, Complete Rslts, Gen | FICR_AR050001UV01 |
| Receiver | Pre-Det Mgr, Complete Rslts, Gen | FICR_AR052001UV01 |
The sender sends a Pre-Determination Query message to determine the status of a previously submitted Pre-Determination Request for medical services and/or products rendered by a physician.
Query response uses the Pre-Determination Results message.
| Trigger Event | Pre-Determination Query Request | QUCR_TE540101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Pre-Determination Event Query Request | QUCR_MT540101UV01 |
| Reason | Trigger Event | Interaction |
| Pre-Determination Query Response | QUCR_TE550101UV01 | QUCR_IN550107UV01 |
| Sender | Pre-Det Rqstr, Comp Rslts, Physician | FICR_AR050007UV03 |
| Receiver | Pre-Det Mgr, Comp Rslts, Physician | FICR_AR052007UV03 |
The sender sends a Pre-Determination Query message to determine the status of a previously submitted Pre-Determination Request for Preferred Accommodation services and/or products.
Query response uses the Pre-Determination Results message.
| Trigger Event | Pre-Determination Query Request | QUCR_TE540101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Pre-Determination Event Query Request | QUCR_MT540101UV01 |
| Reason | Trigger Event | Interaction |
| Pre-Determination Query Response | QUCR_TE550101UV01 | QUCR_IN550103UV01 |
| Sender | Pre-Det Rqstr, Comp Rslts, PAccom | FICR_AR050003UV01 |
| Receiver | Pre-Det Mgr, Comp Rslts, PAccom | FICR_AR052003UV01 |
The sender sends a Pre-Determination Results message containing the processing status (e.g. active, complete) and/or results of a Pre-Determination Request for Chiro Physio services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Query Response | QUCR_TE550101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Pre-Determination Event Complete Chiro Physio | FICR_MT510401UV01 |
| Sender | Pre-Det Mgr, Comp Rslts, ChiroPhysio | FICR_AR052004UV02 |
| Receiver | Pre-Det Rqstr, Comp Rslts, ChiroPhysio | FICR_AR050004UV02 |
The sender sends a Pre-Determination Results message containing the processing status (e.g. active, complete) and/or results of a Pre-Determination Request for Generic services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Query Response | QUCR_TE550101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Pre-Determination Event Complete Generic | FICR_MT510101UV01 |
| Sender | Pre-Det Mgr, Complete Rslts, Gen | FICR_AR052001UV01 |
| Receiver | Pre-Det Rqstr, Complete Rslts, Gen | FICR_AR050001UV01 |
The sender sends a Pre-Determination Results message containing the processing status (e.g. active, complete) and/or results of a Pre-Determination Request for Pharmacy services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Query Response | QUCR_TE550101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Pre-Determination Event Complete Pharmacy | FICR_MT510201UV01 |
| Sender | Pre-Det Mgr, Complete Rslts, Rx | FICR_AR052002UV01 |
| Receiver | Pre-Det Rqstr, Complete Rslts, Rx | FICR_AR050002UV01 |
The sender sends a Pre-Determination Results message containing the processing status (e.g. active, complete) and/or results of a Pre-Determination Request for services and / or products rendered by a physician
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Query Response | QUCR_TE550101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Pre-Determination Event Complete Physician | FICR_MT510701UV03 |
| Sender | Pre-Det Mgr, Comp Rslts, Physician | FICR_AR052007UV03 |
| Receiver | Pre-Det Rqstr, Comp Rslts, Physician | FICR_AR050007UV03 |
The sender sends a Pre-Determination Results message containing the processing status (e.g. active, complete) and/or results of a Pre-Determination Request for Preferred Accommodation services and/or products.
Pre-Determination Results indicate adjudication results for specified services and/or products, but does not generate a payment.
| Trigger Event | Pre-Determination Query Response | QUCR_TE550101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Pre-Determination Event Complete Pref Accom | FICR_MT510301UV01 |
| Sender | Pre-Det Mgr, Comp Rslts, PAccom | FICR_AR052003UV01 |
| Receiver | Pre-Det Rqstr, Comp Rslts, PAccom | FICR_AR050003UV01 |
| Return to top of page |

