|
||||||||||||||||||||||||||
|
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
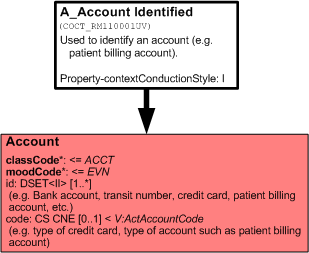
The Account CMET is used to identify account information.
This is the identified variant of A_Account universal
| A_Account identified | COCT_MT110001UV01 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
Note: This CMET replaces or revises material in the HL7 V3 2005 Normative Edition standard. It will appear in the HL7 V3 2006 Normative Edition.
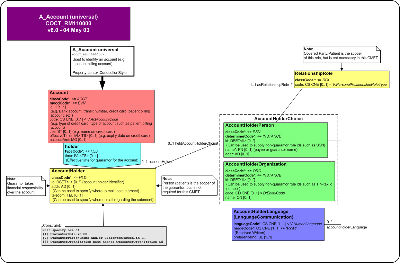
The Account CMET is used to identify account information. An account is an accumulator of financial transactions (e.g. charges, debits, credits) that have either a positive or negative affect on the balance of the account. Examples of accounts are patient billing accounts, cash, credit card, Payor accounts and Payee accounts.
This CMET describes the account, type of account, effective dates for the account (e.g. for credit cards, the start/end dates), an account name (e.g. name on the credit card) and balance.
The account holder is noted, which could either be an individual or organization. If the account holder is a person, it may be useful to note the language that the account holder is conversant in.
| A_Account universal | COCT_MT110000UV04 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
Note: This CMET replaces or revises material in the HL7 V3 2005 Normative Edition standard. It will appear in the HL7 V3 2006 Normative Edition.
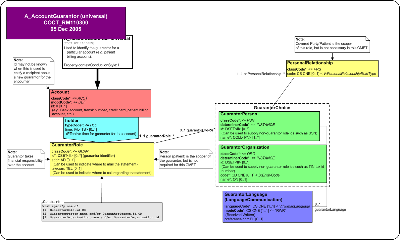
The AccountGuarantor CMET is used to identify the guarantor for a particular account (e.g. patient billing account). A guarantor takes financial responsibility over the account.
This CMET describes the account, type of account, effective dates for the account (e.g. for credit cards, the start/end dates), an account name (e.g. name on the credit card) and balance.
The account holder is noted as the guarantor, which could either be an individual or organization. If the account holder is a person, it may be useful to note the language that the account holder is conversant in. The person that scopes the guarantor (e.g. patient) may also be noted.
| A_AccountGuarantor universal | COCT_MT110300UV04 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
Note: This CMET will appear in the HL7 V3 2006 Normative Edition.
This is the basic variant of A_AccountPayee universal. It is a set of minimal constaints upon the universal CMET.
| A_AccountPayee basic | COCT_MT110202UV04 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
Note: This CMET will appear in the HL7 V3 2006 Normative Edition.
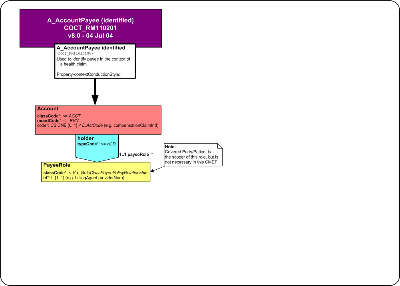
This is the identified variant of A_AccountPayee universal
| A_AccountPayee identified | COCT_MT110201UV04 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
Note: This CMET replaces or revises material in the HL7 V3 2005 Normative Edition standard. It will appear in the HL7 V3 2006 Normative Edition.
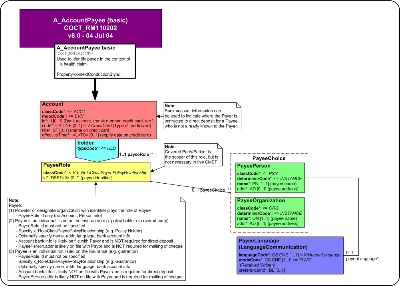
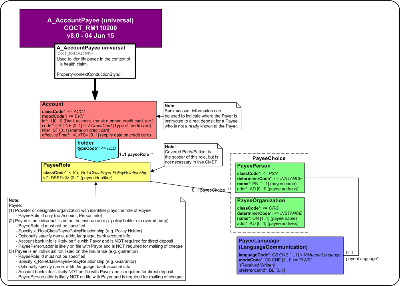
The AccountPayee CMET specifies the Payee, in the context of an Invoice. A Payee is a person or organization that receives payment for services rendered and/or goods provided and receives payment on behalf of one or more Providers. As well, a Payee may be a person who has directly paid the Provider and is being reimbursed by the Payor. In some cases, a Payee may be the same as the Provider.
A Payee is specified in either of 3 ways:
-
[1] Payee is a known entity and has an identifier (e.g. Provider or designate organization).
In this case, only a Payee identifier is specified.
-
[2] Payee is an individual listed on the insurance policy (e.g. policy holder or covered party).
In this case, a Payee identifier is not specified. In its place would be a relationship code from the Payee to the policy (e.g. Policy Holder). Optional information would be Payee name, address, language and bank account information. Note that bank account information and address may be not on file with the Payor.
-
[3] Payee is an individual not listed on the insurance policy (e.g. guarantor).
In this case, a Payee identifier is not specified. In its place would be a relationship code from the Payee to the policy (e.g. Guarantor). Optional information would be Payee name, address, language and bank account information. Note that bank account information and address are likely not on file with the Payor.
| A_AccountPayee universal | COCT_MT110200UV04 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
Note: This CMET will appear in the HL7 V3 2006 Normative Edition.
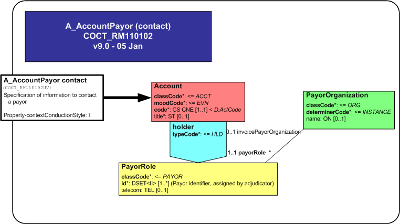
This is the contact variant of A_AccountPayor universal.
| A_AccountPayor contact | COCT_MT110102UV04 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
Note: This CMET will appear in the HL7 V3 2006 Normative Edition.
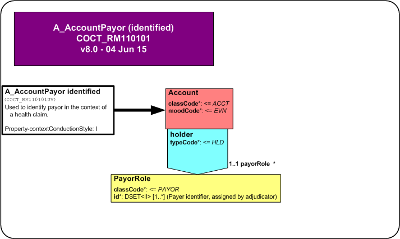
This is the identified variant of A_AccountPayor universal
| A_AccountPayor identified | COCT_MT110101UV04 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
Note: This CMET replaces or revises material in the HL7 V3 2005 Normative Edition standard. It will appear in the HL7 V3 2006 Normative Edition.
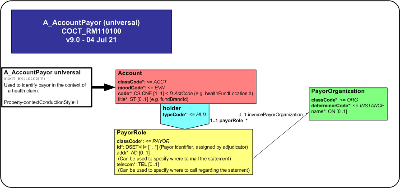
The AccountPayor CMET contains the Payor's identifier. It is used to identify the Payor in the context of an Invoice. A Payor is an organization that establishes benefit/insurance plans, determines eligibility for benefits and funds payment for Goods and/or Services provided to a Person. A Payor may retain a TPA (Third Party Administrator) or Adjudicator to perform some or all of the invoice validation, adjudication and payment. Fundamentally, a Payor is the organization that pays the adjudicated invoice.
| A_AccountPayor universal | COCT_MT110100UV04 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
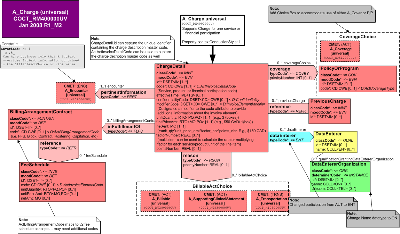
Overview:
The A_Charge (universal) CMET supports the conveyance of invoiced charges relating to a single billable act that is being or has been provided, as indicated by the moodCode EVN.
ChargeDetail
The ChargeDetail is conveyed with the classCode INVE for invoice.
A set of one or more ChargeDetail identifier is required to be sent if available to uniquely identify the invoice in one or more accounting systems.
The ChargeDetail code, which is required to be specified by ActInvoiceDetailCode value set, provides specific information related to the type of billable act provided, e.g., the type of service provided or the type of product dispensed, or the type of financial participation incurred on the part of the guarantor for the billable act.
The ChargeDetail effectiveTime denotes the time period of the billable acts referenced by the ChargeDetail.
The ChargeDetail confidentialityCode may be sent to control the collection, access, and use of information related to this charge. The level of confidentiality is conveyed by a coded concept from the Confidentiality vocabulary domain, which includes codes indicating the types of permitted access, restriction on access, reasons for confidentiality, such as celebrity status of patient, and types of sensitive services or health condition information that requires privacy protection.
The ChargeDetail modifierCode designates a modifier to the code attribute to provide additional information about the invoice element.
The ChargeDetail unitQuantity conveys the ratio of units per service provision or product dispense, e.g., 2 hour session of physical therapy or 3 boxes of a product per dispense.
The ChargeDetail unitPriceAmt conveys the price per unit, e.g., $50 CAD/1{box} or $100 per hour of physical therapy.
The ChargeDetail netAmt is expressed using a currency {the unit in which monetary amounts are denominated in different economic regions] to express the net amount charged based on the product of applicable ChargeDetail unity quantity, unitPriceAmt, factorNumber and pointsNumber attributes.
The ChargeDetail factorNumber is the multiplier or percentage used to calculate the rate for each unitQuantity/unitPriceAmt expressed with a Real integer, e.g., the tax rate.
The ChargeDetail pointsNumber is used where the netAmt is expressed in 'points', this expresses the weighting (based on difficulty, cost and/or resource intensiveness) associated with the good or service delivered.
Links to Other Acts
A ChargeDetail may link to other acts:
Coverage for the billable act by one or more policies or programs may be conveyed using the Coverage COVBY ActRelationship association to one or more PolicyOrProgram or A_Coverage CMET. Coordination of benefits among several PolicyOrPrograms may be conveyed in priorityNumber in terms of the priority of their responsibility for coverage.
A PolicyOrProgram is represented by the classCode COV. An identifier id is required to be sent if available. It is required to be fully specified by a policy or program type from the codeActCoverageTypeCode.
The reference ActRelationship REFR may be used to associate zero or more previouse charges to a ChargeDetail.
The PreviousCharge classCode INVE indicates that this is an invoice.
The PreviousCharge moodCode EVN indicates that an instance of a previous charge invoice actually happened.
The PreviousCharge id ione or more unique identifiers is required to be sent if available.
The author AUT participation may be used to associate one or more DataEnterer with the ChargeDetail. The DataEnterRole is represented by the qualified entityclassCode QUAL. The DataEnterer id is required to be sent if available and the DataEnterer name may be sent.
A DataEntererOrganization may scope the DataEntererRole. This is an organization entity instance with one or more required identifier, and optional name and telecom.
The reason RSON ActRelationship associates a choice of Billable Acts as reasons for the charge. The RSON priorityNumber allows the charges to be prioritized for coding and billing purposes.
The BillableActChoice box enables a choice of the following CMETs to convey information related to clinical or non-clinical acts: A_Billable universal, A_SupportingClinicalInformation universal, A_Transportation universal , or the A_Observation universal. In the future, other Acts or CMETs drawn from electronic provider health records (EHR) may be included in this choice box, which would support conveyance of charge information based on EHR systems.
The inFullfillmentOf ActRelationship associates the ChargeDetail with the BillingArrangementContract, a financial contract expressed with the classCode FCNTCT in definition mood DEF.
The BillingArrangementContract code provides specific information about the type of financial contract with a coded concept from the ActBillingArrangementCode value set, e.g., fee-for-service, capitation, block grant, etc.
The BillingArrangementContract id is required to be sent if available to identify the contract.
The reference REFR ActRelationship associates the BillingArrangementContract with the FeeSchedule expressed with the classCode INVE in definition mode.
The FeeSchedule id is required be sent if available to uniquely identify a fee schedule.
The FeeSchedule code from the ActInvoiceElementCode value set provides specific information about the type of charges that may be invoiced.
The FeeSchedule may carry unitQuantity, unitPriceAmt, and netAmt if these are different or more informative than those carried in the ChargeDetail.
The pertinentInformation ActRelationship typeCode PERTassociates the A_Encounter universal with the ChargeDetail. New in this ballot: The contextControlCode has been removed, because it does not support bi-directional overrides of the patient information. One can have a business rule that R_Patient in A_Encounter overrides patient information contained in the BillableActChoice and vice versa.
| A_EncounterUniversal | COCT_MT010000UV01 |
| A_TransportationUniversal | COCT_MT060000UV01 |
| A_BillableUniversal | COCT_MT280000UV04 |
| A_CoverageUniversal | COCT_MT510000UV06 |
| A_SupportingClinicalStatementUniversal | COCT_MT530000UV |
| A_Charge universal | COCT_MT400000UV07 |
| Parent: | Patient Billing Account (FIAB_DM000000UV) |
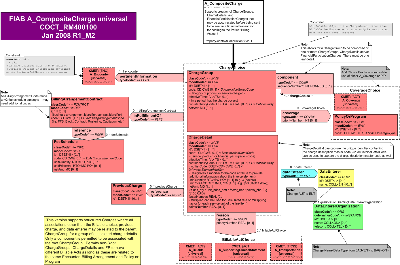
Overview: .
The A_CompositeCharge (universal) CMET supports the conveyance of groups of invoiced charges relating to one or more billable act that is being or has been provided, as indicated by the moodCode EVN. These may be a series of components, which may be other charge groups or charge details. The initial group is the root group. Child groups are nodes, and all paths must end with a charge detail. The various associated classes may either be linked at the group or detail levels, or are restricted to either the group or the detail level.
The focal class is the ChargeGroup which is conveyed with the the classCode for invoice (INVE).
ChargeGroup Attributes
One or more ChargeGroup id is required to identify the ChargeGroup instance.
The ChargeGroup code, which is specified by the ActInvoiceGroupCode, is the category of billable acts charges as conveyed by one or more component ChargeGroups or ChargeDetails.
The ChargeGroup effectiveTime denotes the time period of the billable acts referenced by the ChargeGroup.
The ChargeGroup confidentialityCode is used to control the collection, access, and use of information related to this charge group. The level of confidentiality is conveyed by a coded concept from the Confidentiality vocabulary domain, which includes codes indicating the types of permitted access, restriction on access, reasons for confidentiality, such as celebrity status of patient, and types of sensitive services or health condition information that requires privacy protection. The confidentiality code selected at the ChargeGroup level may be overridden by the confidentiality code selected at the ChargeDetail level.
The ChargeGroup netAmt conveys the total of the amounts charged for each component ChargeDetail.
The focal act ChargeGroup is the root group, which must be a composite of either one or more ChargeGroup or one or more ChargeDetails. The composition is conveyed using the component ActRelationship with a sequenceNumber for structuring the hierarchy, i.e., ordering the elements from the parent groups to the detail elements.
The ChargeDetail is conveyed with the classCode for invoice (INVE).
ChargeDetail Attributes
A set of one or more ChargeDetail identifiers may be used to uniquely identify the invoice in one or more accounting systems.
The ChargeDetail code, which is specified by ActInvoiceDetailCode vocabulary domain, provides specific information related to the type of billable act provided, e.g., the type of service provided or the type of product dispensed, or the type of financial participation incurred on the part of the guarantor for the billable act.
The ChargeDetail effectiveTime denotes the time period of the billable acts referenced by the ChargeDetail.
The ChargeDetail modifierCode designates a modifier to the code attribute to provide additional information about the invoice element, e.g., body site codes or organ donor or how the service was performed.
The ChargeDetail unitQuantity conveys the ratio of units per service provision or product dispense, e.g., 2 hour session of physical therapy or 3 boxes of a product per dispense.
The ChargeDetail unitPriceAmt conveys the price per unit, e.g., $50 CAD/1{box} or $100 per hour of physical therapy.
The ChargeDetail netAmt is expressed using a currency {the unit in which monetary amounts are denominated in different economic regions] to express the net amount charged based on the product of applicable ChargeDetail unity quantity, unityPriceAmt, factorNumber and pointsNumber attributes.
The ChargeDetail factorNumber is the multiplier or percentage used to calculate the rate for each unitQuanitity/unitPriceAmt expressed with a Real integer, e.g., the tax rate.
The ChargeDetail pointsNumber is used where the netAmount is expressed in 'points', this expresses the weighting (based on difficulty, cost and/or resource intensiveness) associated with the good or service delivered.
Links to Other Acts
A ChargeDetail may link to other acts:
Coverage for the billable act by one or more policies or programs may be conveyed using the Coverage (COVBY) association to one or more PolicyOrProgram or A_Coverage CMET. Coordination of benefits among several PolicyOrPrograms may be conveyed in sequenceNumber in terms of the priority of their responsibility for coverage.
A PolicyOrProgram is represented by the classCode COV. It may have an id. It is fully specified by a policy or program type from the code vocabulary domain ActCoverageTypeCode.
The author participation may be used to associate one or more DataEnterer with the ChargeDetail. The DataEnterRole is represented by the qualified entityclassCode QUAL. The DataEnterer id is required and the DataEnterer name is optional.
A DataEntererOrganization may scope the DataEntererRole. This is an organization entity instance with one or more required identifier, name and telecom.
The reasonActRelationship associates a choice of Billable Acts as reasons for the charge only to a ChargeDetail. The reason contextControlCode is valued as additive, propagating and the contextConductionInd has default value of "true". This enables context conduction of the R_Patient from the A_Encounter through to the BillableAct, and overrides any patient role information that may be carried therein. The RSON priorityNumber allows the charges to be prioritized for coding and billing purposes.
The BillableActChoice box enables a choice of the following CMETs to convey information related to clinical or non-clinical acts: A_Billable (universal), A_SupportingClinicalInformation (universal), A_Transportation (universal) or the A_Observation (universal). In the future, other Acts or CMETs drawn from electronic provider health records (HER) may be included in this choice box, which would support conveyance of charge information based on HER systems.
The referenceActRelationship may associate the ChargeGroup or ChargeDetail with a previousCharge ChargeGroup or ChargeDetail. One or more identifiers are required.
The inFullfillmentOfActRelationship associates the ChargeGroup or ChargeDetail with the BillingArrangementContract , a financial contract expressed with the classCode FCNTCT.
The BillingArrangementContract code provides specific information about the type of financial contract with a coded concept from the ActBillingArrangementCode vocabulary domain, e.g., fee-for-service, capitation, block grant, etc.
The reference ActRelationship associates the BillingArrangementContract with the FeeSchedule expressed with the Act.classCode INV in definition mode.
The FeeSchedule id may be used to identify an item in a fee schedule.
The FeeSchedule code ActInvoiceElementCode provides specific information about the type of charges that may be invoiced.
The FeeSchedule may carry unitQuantity, unitPriceAmt, and netAmt if these are different or more informative than those carried in the ChargeDetail.
The pertinentInformation ActRelationship typeCode PERTassociates the A_Encounter universal with the ChargeDetail. New in this ballot: The contextControlCode has been removed, because it does not support bi-directional overrides of the patient information. One can have a business rule that R_Patient in A_Encounter overrides patient information contained in the BillableActChoice and vice versa.
| A_EncounterUniversal | COCT_MT010000UV01 |
| A_TransportationUniversal | COCT_MT060000UV01 |
| A_BillableUniversal | COCT_MT280000UV04 |
| A_CoverageUniversal | COCT_MT510000UV06 |
| A_SupportingClinicalStatementUniversal | COCT_MT530000UV |
| A_CompositeCharge universal | COCT_MT400100UV07 |
| Return to top of page |

