Accounting and Billing
 ANSI/HL7 V3 AB, R2-2008 (R2012) HL7 Version 3 Standard: Accounting and Billing, Release 2 03/06/2008 (reaffirmed 6/5/2012) |
| Responsible Group | Financial Management Work Group HL7 |
| Financial Management Co-Chair + Vocabulary Facilitator + Modeling Facilitator | Kathleen Connor Fox Systems, Inc. |
| Financial Management Co-Chair + V2 and Mapping Expert | Susan Lepping Siemens Medical Solutions |
| Financial Management Co-Chair + Mapping Expert | Francine Kitchen IDX Systems Corporation |
| Recent Past Financial Management Co-Chair | Michael van Campen Gordon Point Informatics Ltd. - HL7 Canada |
| Primary Contributor | Mark Shafarman Shafarman Consulting |
| Contributor | Lloyd McKenzie Lloyd McKenzie and Associates - HL7 Canada |
HTML Generated: 2012-08-31T12:06:42
Content Last Edited: 2008-06-04T13:47:15
HL7® Version 3 Standard, © 2008 Health Level Seven® International All Rights Reserved.
HL7 and Health Level Seven are registered trademarks of Health Level Seven International. Reg. U.S. Pat & TM Off.
Use of these materials is governed by HL7 International's IP Compliance Policy.
Table of Contents
Preface
i Notes to Readers
ii Message Design Element Navigation
1 Overview
1.1 Introduction & Scope
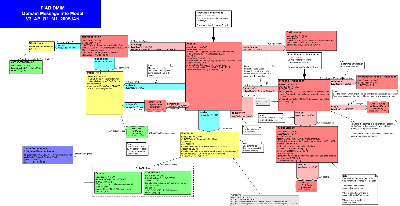
1.2 Domain Information Models
2 Patient Billing Account Topic
2.1 Introduction
2.2 Storyboards
2.3 Application Roles
2.4 Trigger Events
2.5 Refined Message Information Models
2.6 Hierarchical Message Descriptions
2.7 Interactions
3 Patient Billing Post Topic
3.1 Introduction
3.2 Storyboards
3.3 Application Roles
3.4 Trigger Events
3.5 Refined Message Information Models
3.6 Hierarchical Message Descriptions
3.7 Interactions
4 Quality Analysis Report Topic
5 CMETs Defined by this Domain
6 Interactions Annex
6.1 By Application Role
6.2 By Trigger Event
6.3 By Message Type
7 Glossary
This is release 2 of the Account and Billing domain. This content passed normative ballot during the September 2007 ballot cycle and was subsequently approved as an ANSI standard.
FOR INFORMATIONAL PURPOSES ONLY: The following link is to an excel spreadsheet containing data mapping from HL7 Version 2.5 Chapter 6 to HL7 V3 FIAB: V2 - V3 Mapping Document.
The spreadsheet contains a separate worksheet for each version 2.5 Chapter 6 segment. This V2-V3 mapping in not intended to be balloted or to become normative. In is included in the hope that it will be helpful for implementations. The FM work group welcomes any geedback, questions or corrections. Please send any feedback to francine.kitchen@ge.com.
|
||||||
|
The Accounting and Billing (AB) domain covers the creation and management of patient billing accounts, primarily for the purpose of collecting charges and credits (financial transactions) to support the submission of a claim or invoice for reimbursement.
| Return to top of page |