 ANSI/HL7 V3 CR, R4-2008 HL7 Version 3 Standard: Claims and Reimbursement, Release 4 02/20/2008 |
Content Last Edited: 2009-09-04T22:38:52
8.2 Storyboards
8.3 Application Roles
8.4 Trigger Events
8.5 Refined Message Information Models
8.6 Hierarchical Message Descriptions
8.7 Interactions
The Statement of Financial Activity or SOFA queries allows the Provider application to reconcile with the Adjudicator. This may be necessary over time when the Provider application and Adjudicator application have made different interpretations of what monies are owed to a Payee (or their agent).
|
||||||||||||||||
|
For details on the interpretation of this section, see the storyboard discussion in the Version 3 Guide.
To demonstrate how a query for SOFA Detail information is generated and submitted. A request for Account Details, in the event that a discrepancy has occurred, yields a response that contains a complete record of each transaction within the defined group of transactions identified by the Provider.
| SOFA Detail Query Request, Gen | |
| SOFA Detail Query Results, Gen |
Bender Clinic maintains standard office hours and procedures. As part of the Clinic's end of day procedures, Account Summaries are requested from each Payor for the current business day and compared to an internal report generated from the practice management application.
Upon closing on Monday December 17, 2001, the Chiropractor on duty generates an internal summary report for each of the Payors with which the Clinic does business. The date selected for these reports is December 17, 2001. These are set aside. He then requests an Account Summary from each Payor noting December 17, 2001 as the adjudication date. Below is a depiction of the response received from one of the Payors. Please note the Clinic's practice management application stores the Account Summary Response and offers the user the option to view the file or have it print to paper. The Chiropractor, as a rule, always prints the file.
Account Summary - Bender Clinic
Adjudication Date: December 17, 2001
Payor: HC Payor, Inc.
-
Number of Invoices Processed: 125
-
Total Dollar Value: $2,536.25
-
Number of Same Day reversals: 2
-
Value of Same Day reversals: $15.05
-
Number of Prior Reversals: 0
-
Value of Prior Reversals: $0.00
-
Number of Rejected Items: 0
-
Value of Rejected Items: $0.00
-
Number of Pay Patient Items: 0
-
Value of Pay Patient Items: $0.00
-
Net Invoices Processed: 123
-
Net Dollar Value: $2,521.20
The Chiropractor then compares the values noted on the Account Summary report to the values noted on the internal report for the same Payor. He notices that the values don't match. The internal report notes a net of 122 Invoices processed with a dollar value of $2,395.75. There is one Invoice valued at $125.45 not accounted for. As the alarm company is already calling, the Chiropractor decides to set this aside to rectify tomorrow.
Upon his arrival on Tuesday December 18, 2001, the Chiropractor first generates an internal detail report that notes details of the 122 Invoices processed by HC Payor, Inc. December 17, 2001. He then requests an Account Detail from the Payor for the adjudication date of December 17, 2001. Again, his application offers him the choice to either view the file on the screen or print a copy. He elects to print a copy.
As both reports are sorted by Invoice number, he quickly compares the two and discovers that there is one Invoice noted on the Account Detail report that is not noted on his internal detail report. This Invoice happens to have a value of $125.45 associated with it. The Chiropractor then enters the Invoice number into his practice management application.
This exercise reveals that the system never received a response from the Payor for that particular Invoice. This explains why it was never included on the internal summary and detail reports.
The Chiropractor contacts HC Payor's Provider call centre. He provides the call centre representative with the required information. The rep reviews the Invoice and discovers that the Adjudication Response for the Invoice was generated, however, it was never received by the Provider due to a momentary network problem. So instead of throwing the Adjudication Results away, the Payor placed the Adjudication Results on a queue for the Provider. Despite this, the system still considered the Invoice to have been successfully processed and thus why the Account Summary and Detail responses included it. The call centre rep instructs the Chiropractor to poll the queue (to get the missing Adjudication Results) and re-run his reports.
The Chiropractor does as he is instructed. Upon re-processing his reports, all of the values reconcile.
To demonstrate how a query for SOFA Detail information is generated and submitted. A request for Account Details, in the event that a discrepancy has occurred, yields a response that contains a complete record of each transaction within the defined group of transactions identified by the Provider.
| SOFA Detail Query Request, Rx | |
| SOFA Detail Query Results, Rx |
Good Neighbor Pharmacy is a typical drug store operation with stable hours of operation. The hours of operation are as follows:
-
Monday to Friday: 9am to 9pm
-
Saturday: 9am to 6pm
-
Sundays and holidays: 11am to 5pm
As part of the pharmacy's end of day procedures, Account Summaries are requested from each Payor for the current business day and compared to an internal report generated from the practice management application.
Upon closing on Monday December 17, 2001, the pharmacist on duty generates an internal summary report for each of the Payors that the pharmacy does business with. The date selected for these reports is December 17, 2001. These are set aside. He then requests an Account Summary from each Payor noting December 17, 2001 as the adjudication date. Below is a depiction of the response received from one of the Payors. Please note the pharmacy's practice management application stores the Account Summary Response and offers the pharmacist/user the option to view the file or have it print to paper. The pharmacist, as a rule, always prints the file.
Account Summary - Good Neighbor Pharmacy
Adjudication Date: December 17, 2001
Payor: HC Payor, Inc.
-
Number of Invoices Processed: 125
-
Total Dollar Value: $2,536.25
-
Number of Same Day reversals: 2
-
Value of Same Day reversals: $15.05
-
Number of Prior Reversals: 0
-
Value of Prior Reversals: $0.00
-
Number of Rejected Items: 0
-
Value of Rejected Items: $0.00
-
Number of Pay Patient Items: 0
-
Value of Pay Patient Items: $0.00
-
Net Invoices Processed: 123
-
Net Dollar Value: $2,521.20
The pharmacist then compares the values noted on the Account Summary report to the values noted on the internal report for the same Payor. He notices that the values don't match. The internal report notes a net of 122 Invoices processed with a dollar value of $2,395.75. There is one Invoice valued at $125.45 not accounted for. As the alarm company is already calling, the pharmacist decides to set this aside to rectify tomorrow.
Upon his arrival on Tuesday December 18, 2001, the pharmacist first generates an internal detail report that notes details of the 122 Invoices processed by HC Payor, Inc. on December 17, 2001. He then requests an Account Detail from the Payor for the adjudication date of December 17, 2001. Again, his application offers him the choice to either view the file on the screen or print a copy. He elects to print a copy.
As both reports are sorted by Invoice number, he quickly compares the two and discovers that there is one Invoice noted on the Account Detail report that is not noted on his internal detail report. This Invoice happens to have a value of $125.45 associated with it. The pharmacist then enters the Invoice number into his practice management application. This exercise reveals that the system never received a response from the Payor for that particular Invoice. This explains why it was never included on the internal summary and detail reports.
The pharmacist contacts the HC Payor's Provider call centre. He provides the call centre representative with the required information. The rep reviews the Invoice and discovers that the Adjudication Response for the Invoice was generated, however, it was never received by the Provider due to a momentary network problem. So instead of throwing the Adjudication Results away, the Payor placed the Adjudication Results on a queue for the Provider. Despite this, the system still considered the Invoice to have been successfully processed and thus why the Account Summary and Detail responses included it. The call centre rep instructs the pharmacist to poll the queue (to get the missing Adjudication Results) and re-run his reports.
The pharmacist does as he is instructed. Upon re-processing his reports, all of the values reconcile.
To demonstrate how a query for SOFA Detail information is generated and submitted. A request for Account Details, in the event that a discrepancy has occurred, yields a response that contains a complete record of each transaction within the defined group of transactions identified by the Provider.
As part of the Good Health Hospital Billing Department's end of week procedures, Account Summaries are requested from the Insurers for the Preferred Accommodation Invoices submitted during the week. These are compared to an internal report generated from the hospital's financial management application. Below are the results from a request for an Account Summary Detail from HC Payor, Inc.
Preferred Accomodation Account Summary - Good Health Hospital
Invoice Dates: January 11, 2002 - January 17, 2002
Payor: HC Payor, Inc.
-
Number of Invoices Processed: 125
-
Total Dollar Value: $52,250.00
-
Number of Same Day reversals: 2
-
Value of Same Day reversals: $550.00
-
Number of Prior Reversals: 0
-
Value of Prior Reversals: $0.00
-
Number of Rejected Items: 0
-
Value of Rejected Items: $0.00
-
Number of Pay Patient Items: 0
-
Value of Pay Patient Items: $0.00
-
Net Invoices Processed: 123
-
Net Dollar Value: $51,700.00
The accounting clerk compares the values on the Account Summary report to the values noted on the internal report for the same Payor. He notices the values do not match. The internal report notes a net of 122 Invoices processed with a dollar value of $50,250.00. There is one Invoice valued at $450.00 for two semi-private rooms not accounted for. The clerk first generates an internal detail report that notes details of the 122 Invoices processed by HC Payor, Inc. He then requests an Account Detail from the Payor for the adjudication date of January 14, 2002. Again, his application offers him the choice to either view the file on the screen or print a copy. He elects to print a copy.
As both reports are in Invoice Number sequence, he quickly compares the two and discovers that there is one Invoice noted on the Account Detail report not listed on his internal detail report. This Invoice happens to have a value of $450.00 associated with it. The clerk enters the Invoice number into his financial management application. This exercise reveals the system never received a response from the Payor for that particular Invoice. This explains why it was never included on the internal summary and detail reports.
The accounting clerk contacts the Payor's Provider call centre. He provides the call centre representative with the required information. The rep reviews the Invoice and discovers that the Adjudication Response for the Invoice was generated, however, the Provider, due to a momentary network problem, never received it. So instead of throwing the Adjudication Results away, the Payor placed the Adjudication Results on a queue for the Provider. Despite this, the system still considered the Invoice to have been successfully processed and thus why the Account Summary and Detail responses included it. The call centre rep instructs the accounting clerk to poll the queue (to get the missing Adjudication Results) and re-run his reports.
Following the poll, the accounting clerk re-processes his reports, all of the values reconcile.
To demonstrate how a query for SOFA Summary information is generated and submitted. This is a request for daily totals for Provider and / or insured transactions received, accepted, rejected or reversed. The response provides the daily total payable as well as a breakdown for the transaction types that have occurred on the date indicated.
| SOFA Pymt Adv Query Request, Gen | |
| SOFA Pymt Adv Query Results, Gen |
Bender Clinic maintains standard office hours and procedures. As part of the Clinic's end of day procedures, Account Summaries are requested from each Payor for the current business day and compared to an internal report generated from the practice management application.
Upon closing on Monday December 17, 2001, the Chiropractor on duty generates an internal summary report for each of the Payors with which the Clinic does business. The date selected for these reports is December 17, 2001. These are set aside. He then requests an Account Summary from each Payor noting December 17, 2001 as the adjudication date. Below is a depiction of the response received from one of the Payors. Please note the Clinic's practice management application stores the Account Summary Response and offers the user the option to view the file or have it print to paper. The Chiropractor, as a rule, always prints the file.
Account Summary - Bender Clinic
Adjudication Date: December 17, 2001
Payor: HC Payor, Inc.,
-
Number of Invoices Processed: 125
-
Total Dollar Value: $2,536.25
-
Number of Same Day reversals: 2
-
Value of Same Day reversals: $15.05
-
Number of Prior Reversals: 0
-
Value of Prior Reversals: $0.00
-
Number of Rejected Items: 0
-
Value of Rejected Items: $0.00
-
Number of Pay Patient Items: 0
-
Value of Pay Patient Items: $0.00
-
Net Invoices Processed: 123
-
Net Dollar Value: $2,521.20
The Chiropractor then compares the values noted on the Account Summary report to the values noted on the internal report for the same Payor. Everything balances and he goes home for the evening.
To demonstrate how a query for SOFA Summary information is generated and submitted. This is a request for daily totals for Provider and / or insured transactions received, accepted, rejected or reversed. The response provides the daily total payable as well as a breakdown for the transaction types that have occurred on the date indicated.
| SOFA Pymt Adv Query Request, Rx | |
| SOFA Pymt Adv Query Results, Rx |
Good Neighbor Pharmacy is a typical drug store operation with stable hours of operation. The hours of operation are as follows:
-
Monday to Friday: 9am to 9pm
-
Saturday: 9am to 6pm
-
Sundays and holidays: 11am to 5pm
As part of the pharmacy's end of day procedures, Account Summaries are requested from each Payor for the current business day and compared to an internal report generated from the practice management application.
Upon closing on Monday December 17, 2001, the pharmacist on duty generates an internal summary report for each of the Payors that the pharmacy does business with. The date selected for these reports is December 17, 2001. These are set aside. He then requests an Account Summary from each Payor noting December 17, 2001 as the adjudication date. Below is a depiction of the response received from one of the Payors. Please note the pharmacy's practice management application stores the Account Summary Response and offers the pharmacist/user the option to view the file or have it print to paper. The pharmacist, as a rule, always prints the file.
Account Summary - Good Neighbor Pharmacy
Adjudication Date: December 17, 2001
Payor: HC Payor, Inc.
-
Number of Invoices Processed: 125
-
Total Dollar Value: $2,536.25
-
Number of Same Day reversals: 2
-
Value of Same Day reversals: $15.05
-
Number of Prior Reversals: 0
-
Value of Prior Reversals: $0.00
-
Number of Rejected Items: 0
-
Value of Rejected Items: $0.00
-
Number of Pay Patient Items: 0
-
Value of Pay Patient Items: $0.00
-
Net Invoices Processed: 123
-
Net Dollar Value: $2,521.20
To demonstrate how a query for SOFA Summary information is generated and submitted. This is a request for daily totals for Provider and / or insured transactions received, accepted, rejected or reversed. The response provides the daily total payable as well as a breakdown for the transaction types that have occurred on the date indicated.
As part of the Good Health Hospital Billing Department's end of week procedures, Account Summaries are requested from the Insurers for the Preferred Accommodation Invoices submitted during the week. These are compared to an internal report generated from the hospital's financial management application. The Query submitted to the Insurer includes the Hospital Account Number, and the first submission date of the query. On Friday, the billing department requests an Account Summary for the past week's invoice submissions.
Below is a depiction of the response received from one of the Insurers. The hospital's financial management application stores the Account Summary Response and offers the billing clerk the option to view the file or have it print to paper.
Preferred Accomodation Account Summary - Good Health Hospital
Invoice Dates: January 11, 2002 - January 17, 2002
Payor: HC Payor, Inc.
-
Number of Invoices Processed: 125
-
Total Dollar Value: $52,250.00
-
Number of Same Day reversals: 2
-
Value of Same Day reversals: $550.00
-
Number of Prior Reversals: 0
-
Value of Prior Reversals: $0.00
-
Number of Rejected Items: 0
-
Value of Rejected Items: $0.00
-
Number of Pay Patient Items: 0
-
Value of Pay Patient Items: $0.00
-
Net Invoices Processed: 123
-
Net Dollar Value: $51,700.00
|
||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of application roles and their relationships in the Version 3 Guide.
An application that requests financial transaction details for Invoices processed by the SOFA Manager within a specified date range.
SOFA (Statement of Financial Activity) Reports may include transaction totals and dollar amounts for transactions received, accepted, rejected, or cancelled.
An application that requests financial transaction details for Invoices, Generic processed by the SOFA Manager within a specified date range.
SOFA (Statement of Financial Activity) Reports may include transaction totals and dollar amounts for transactions received, accepted, rejected, or cancelled.
An application that requests financial transaction details for Invoices, Pharmacy processed by the SOFA Manager within a specified date range.
SOFA (Statement of Financial Activity) Reports may include transaction totals and dollar amounts for transactions received, accepted, rejected, or cancelled.
An application that requests financial transaction details for Invoices, Preferred Accommodation processed by the SOFA Manager within a specified date range.
SOFA (Statement of Financial Activity) Reports may include transaction totals and dollar amounts for transactions received, accepted, rejected, or cancelled.
An application that responds to a SOFA Request with the Final SOFA Results only.
SOFA (Statement of Financial Activity) Reports may include transaction totals and dollar amounts for transactions received, accepted, rejected, or cancelled.
The Final SOFA Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the SOFA Request by a period of time (perhaps one or more days).
An application that responds to a SOFA Request, Generic with the Final SOFA Results only.
SOFA (Statement of Financial Activity) Reports may include transaction totals and dollar amounts for transactions received, accepted, rejected, or cancelled.
The Final SOFA Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the SOFA Request by a period of time (perhaps one or more days).
An application that responds to a SOFA Request, Pharmacy with the Final SOFA Results only.
SOFA (Statement of Financial Activity) Reports may include transaction totals and dollar amounts for transactions received, accepted, rejected, or cancelled.
The Final SOFA Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the SOFA Request by a period of time (perhaps one or more days).
An application that responds to a SOFA Request, Preferred Accommodation with the Final SOFA Results only.
SOFA (Statement of Financial Activity) Reports may include transaction totals and dollar amounts for transactions received, accepted, rejected, or cancelled.
The Final SOFA Results may arrive close to immediate (i.e. in the same query/response interaction) or may lag the SOFA Request by a period of time (perhaps one or more days).
|
||||||||||||
|
For details on the interpretation of this section, see the discussion of trigger events in the Version 3 Guide.
| Type: | User request |
A trigger to send a SOFA Detail Query to obtain detailed financial activity information for a specified date range.
SOFA (Statement of Financial Activity) Detail totals may include transaction totals and dollar amounts for Invoice received, accepted, rejected or nullified. References to adjudicated Invoices are also included.
| Type: | Interaction based |
A trigger to send a SOFA Detail Query Response with details of financial activity for a Payee.
SOFA (Statement of Financial Activity) details may include transaction totals and dollar amounts for Invoices received, accepted, rejected or nullified. References to adjudicated Invoices are also included.
| Type: | User request |
A trigger to send a SOFA Payment Advice Query to obtain summary financial activity information for a specified date.
SOFA (Statement of Financial Activity) Payment Advice totals will be reported on a future Payment Advice and may include transaction totals and dollar amounts for Invoices received, accepted, rejected or nullified.
| Type: | Interaction based |
A trigger to send a SOFA Payment Advice Query Response with details of financial activity for a Payee.
SOFA (Statement of Financial Activity) Payment Advice totals will be reported on a future Payment Advice and may include transaction totals and dollar amounts for Invoices received, accepted, rejected or nullified.
|
||||||||||||
|
For details on the interpretation of this section, see the description of RMIMs in the Version 3 Guide.
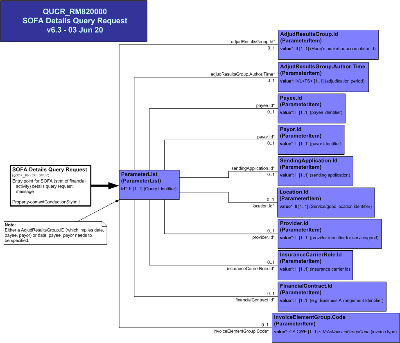
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to send a SOFA Details Query Request message from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
It is used when an out of balance situation has been detected between the Provider receivables and Adjudicator payables. Details of the billable items are requested to aid in identifying the suspected billing discrepancy.
The response is the SOFA Details Query Results message. The details are categorized by Adjudication Result status code state (e.g. acknowledged, pended, rejected, paid etc).
The details are made up of the AdjudResultsGroup supported by the AdjudicatedInvoiceElementGroup, AdjudicationResult and the InvoiceElementGroup references and amounts.
| SOFA Details Query Request | QUCR_HD820100UV01 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to send a SOFA Details Query Results message as a response to a SOFA Details Query Request Request from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
It is used when an out of balance situation has been detected between the Provider receivables and Payor payables. Details of the billable items are presented in the report to aid in identifying the suspected billing discrepancy.
Details are categorized by Adjudication Result status code state (e.g. acknowledged, pended, rejected, paid etc.). The details are made up of the AdjudResultsGroup supported by the AdjudicatedInvoiceElementGroup, AdjudicationResult and the InvoiceElementGroup references and amounts.
| SOFA Details Query Results | QUCR_HD830100UV01 |
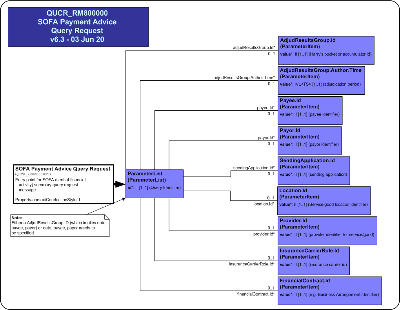
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to send a SOFA (Statement of Financial Activity) Payment Advice Query Request message from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
It is used to request totals for the items submitted for adjudication and payment. This includes counts and amounts for billed items, adjudicated items and paid items.
The query is a set of parameters to limit and group the query results (e.g. AdjudResultsGroup id from a Payment Advice Summary, author, payee, payor, sending application id, location, provider, carrier, contract).
| SOFA Payment Advice Query Request | QUCR_HD800100UV01 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to send a SOFA Payment Advice Query Results message as a response to a SOFA Payment Advice Query Request from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
It is used to indicate totals for the queried specified items that have been submitted for adjudication and payment. This includes counts and amounts for billed items, adjudicated items and paid items (such as Payable Item Count, Total Amount Payable, Number and value of same period reversals, prior reversals, Nullifies, pending and rejected items and the number of adjudicated to zero items and reimbursement items)
It may have subtotals specified for payor, payee, location, business arrangement identifier (contract), provider, carrier, sending application id within the Adjudication Date within the SOFA reporting time range as specified by the AdjudResultsGroup code.
| SOFA Payment Advice Query Results | QUCR_HD810100UV01 |
|
||||||||||||
|
For details on the interpretation of this section, see the description of HMDs in the Version 3 Guide.
This message is used when an out of balance situation has been detected between the Provider receivables and Adjudicator payables. Details of the billable items are presented in the report to aid in identifying the suspected billing discrepancy.
Details are categorized by Adjudication Result status code state (e.g. acknowledged, pended, rejected, paid etc.).
The details are made up of the AdjudResultsGroup supported by the AdjudicatedInvoiceElementGroup, AdjudicationResult and the InvoiceElementGroup references and amounts.
This message is a request to the Payor for Account (Summary) information including the totals for the Payable Item Count, Total Amount Payable, Number and value of same period reversals, prior reversals, Nullifys, pending and rejected items and the number of adjudicated to zero items and reimbursement items.
The result may have subtotals for Business Arrangement Identifier, Provider, Provider Organization, transaction type, Adjudication Date as specified by the AdjudicationGroup code.
The Adjudicator uses this message to respond to the SOFA Payment Advice Query Request indicating the totals for the queried specified items that have been submitted for adjudication and payment. This includes counts and amounts for billed items, adjudicated items and paid items (such as Payable Item Count, Total Amount Payable, Number and value of same period reversals, prior reversals, Nullifies, pending and rejected items and the number of adjudicated to zero items and reimbursement items)
It may have subtotals specified for payor, payee, location, business arrangement identifier (contract), provider, carrier, sending application id within the Adjudication Date within the SOFA reporting date-time range as specified by the AdjudResultsGroup code.
|
||||||||||||||||||||
|
For details on the interpretation of this section, see the definition of Interactions in the Version 3 Guide.
The sender sends a SOFA (Statement of Financial Activity) Detail Query message for Generic services and/or products.
The request is for detailed account activity information, including references to previously adjudicated Invoices.
| Trigger Event | SOFA Detail Query Request | QUCR_TE820101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | SOFA Event Detail Query Request | QUCR_MT820101UV01 |
| Reason | Trigger Event | Interaction |
| SOFA Detail Query Response | QUCR_TE830101UV01 | QUCR_IN830101UV01 |
| Sender | SOFA Rqstr, Gen | FICR_AR080001UV01 |
| Receiver | SOFA Query Mgr, Gen | FICR_AR081001UV01 |
The sender sends a SOFA (Statement of Financial Activity) Detail Query message for Pharmacy services and/or products.
The request is for detailed account activity information, including references to previously adjudicated Invoices.
| Trigger Event | SOFA Detail Query Request | QUCR_TE820101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | SOFA Event Detail Query Request | QUCR_MT820101UV01 |
| Reason | Trigger Event | Interaction |
| SOFA Detail Query Response | QUCR_TE830101UV01 | QUCR_IN830102UV01 |
| Sender | SOFA Rqstr, Rx | FICR_AR080002UV01 |
| Receiver | SOFA Query Mgr, Rx | FICR_AR081002UV01 |
The sender sends a SOFA (Statement of Financial Activity) Detail Query Response message for Generic services and/or products.
The response is for detailed account activity information, including references to previously adjudicated Invoices.
| Trigger Event | SOFA Detail Query Response | QUCR_TE830101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | SOFA Event Payment Advice Query Response | QUCR_MT810101UV01 |
| Sender | SOFA Query Mgr, Gen | FICR_AR081001UV01 |
| Receiver | SOFA Rqstr, Gen | FICR_AR080001UV01 |
The sender sends a SOFA (Statement of Financial Activity) Detail Query Response message for Pharmacy services and/or products.
The response is for detailed account activity information, including references to previously adjudicated Invoices.
| Trigger Event | SOFA Detail Query Response | QUCR_TE830101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | SOFA Event Payment Advice Query Response | QUCR_MT810101UV01 |
| Sender | SOFA Query Mgr, Rx | FICR_AR081002UV01 |
| Receiver | SOFA Rqstr, Rx | FICR_AR080002UV01 |
The sender sends a SOFA (Statement of Financial Activity) Payment Advice Query message for Generic services and/or products.
The request is for summary level account information, including daily totals. Totals will be reported on a future Payment Advice.
| Trigger Event | SOFA Payment Advice Query Request | QUCR_TE800101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | SOFA Event Payment Advice Query Request | QUCR_MT800101UV01 |
| Reason | Trigger Event | Interaction |
| SOFA Payment Advice Query Response | QUCR_TE810101UV01 | QUCR_IN810101UV01 |
| Sender | SOFA Rqstr, Gen | FICR_AR080001UV01 |
| Receiver | SOFA Query Mgr, Gen | FICR_AR081001UV01 |
The sender sends a SOFA (Statement of Financial Activity) Payment Advice Query message for Pharmacy services and/or products.
The request is for summary level account information, including daily totals. Totals will be reported on a future Payment Advice.
| Trigger Event | SOFA Payment Advice Query Request | QUCR_TE800101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | SOFA Event Payment Advice Query Request | QUCR_MT800101UV01 |
| Reason | Trigger Event | Interaction |
| SOFA Payment Advice Query Response | QUCR_TE810101UV01 | QUCR_IN810102UV01 |
| Sender | SOFA Rqstr, Rx | FICR_AR080002UV01 |
| Receiver | SOFA Query Mgr, Rx | FICR_AR081002UV01 |
The sender sends a SOFA (Statement of Financial Activity) Payment Advice Query Response message for Generic services and/or products.
The response include summary level account information, including daily totals. Totals will be reported on a future Payment Advice.
| Trigger Event | SOFA Payment Advice Query Response | QUCR_TE810101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | SOFA Event Payment Advice Query Response | QUCR_MT810101UV01 |
| Sender | SOFA Query Mgr, Gen | FICR_AR081001UV01 |
| Receiver | SOFA Rqstr, Gen | FICR_AR080001UV01 |
The sender sends a SOFA (Statement of Financial Activity) Payment Advice Query Response message for Pharmacy services and/or products.
The response include summary level account information, including daily totals. Totals will be reported on a future Payment Advice.
| Trigger Event | SOFA Payment Advice Query Response | QUCR_TE810101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | SOFA Event Payment Advice Query Response | QUCR_MT810101UV01 |
| Sender | SOFA Query Mgr, Rx | FICR_AR081002UV01 |
| Receiver | SOFA Rqstr, Rx | FICR_AR080002UV01 |
| Return to top of page |

