 ANSI/HL7 V3 CR, R4-2008 HL7 Version 3 Standard: Claims and Reimbursement, Release 4 02/20/2008 |
Content Last Edited: 2009-09-04T22:38:52
2.2 Storyboards
2.3 Application Roles
2.4 Trigger Events
2.5 Refined Message Information Models
2.6 Hierarchical Message Descriptions
2.7 Interactions
Eligibility is a determination by an insurance carrier or designate that a specific insurance policy is in effect on a specific date for a specific individual. It does not imply that a particular service and/or product will be covered and/or paid if submitted to an insurance carrier or designate.
|
||||||||
|
For details on the interpretation of this section, see the storyboard discussion in the Version 3 Guide.
To demonstrate the submission of a query to determine the status of a patient's eligibility for healthcare services. This may impact what services will be rendered to the patient and who will pay for them.
| Elig Query Request, Gen | |
| Elig Query Results, Gen |
During a patient's visit to the optometrist, it was determined that the patient would benefit from the use of eyeglasses. The optometrist asked the patient if they had eyeglass coverage with an extended benefit plan. The patient indicated that they were not sure but that they thought they had some type of extended coverage through their employer with the HC Payor, Inc. The patient looked through their wallet and in fact found an HC Payor, Inc. extended benefit coverage card that included the plan ID, group coverage number, insured's ID number, name and DOB and plan expiry date.
The optometrist asked the patient if they would like the secretary to determine if they were covered by the HC Payor, Inc. extended benefit plan for the purchase of eyeglasses. The patient indicated that they would appreciate this because if eyeglasses were not covered under the plan, they would not be able to purchase them at this time.
The secretary queried the HC Payor, Inc. extended benefit plan giving the patient unique identifier, name, DOB, as well as the plan particulars from the patient benefit coverage card and asked if eyeglasses were covered under the plan for this patient. The response indicated that for this patient and plan, a maximum of $300.00 every 2 years is covered for the purchase of eyeglasses. This was communicated to the patient, who immediately identified they would like to purchase a pair of eyeglasses. It should be noted that the response by the Payor is not a commitment from the Payor to pay for the eyeglasses (the claim).
Mr. Adam Everyman strains his back while at work (Dec 18, 2001) and goes to see his General Practitioner, Dr. Fay Family, who determines the patient should be off work and may benefit from physiotherapy. The doctor's office submits an electronic document to HC Payor, Inc., to establish a claim, then refers Mr. Everyman to the Early Recovery Clinic for treatment.
The Early Recovery Clinic receives a referral and a request for an appointment to treat Mr. Everyman. When asked, he indicated that Dr. Family had submitted an injury report to HC Payor, Inc. but had not yet received any reply or claim number. Mr. Everyman also supplies his Provincial Health Number (ID # 592939). The appointment was made for the next day.
The Early Recovery Clinic office staff then prepared an eligibility message to be sent to HC payor, Inc. to confirm that Mr. Everyman's claim has been accepted by HC Payor, Inc.
The eligibility response indicated that Mr. Everyman's claim had been accepted and his claim number (# 49349) is supplied with the response for future use. Also, it was indicated that a maximum of 8 treatments (fee code of 19160 - single physical therapy visit) would be covered without further authorization (as per the Physio Therapy contract in place).
To demonstrate the submission of a query to determine the status of a patient's eligibility for preferred accommodation services. This may impact what accommodation types are available to the patient and who will pay for them.
| Elig Query Request, PAccom | |
| Elig Query Results, PAccom |
Mrs. Everywoman is expecting a baby, due to be born in July. In February she pre-registers with the hospital for postpartum accommodation and indicates a preference for a private room. She has an extended medical plan through her employer with HC Payor, Inc. She does not know the extent to which her insurer covers hospital accommodation, but submits to the hospital her plan number and employer group number.
The hospital submits a query to HC Payor, Inc. for Mrs. Everywoman's eligibility for preferred accommodation.
The eligibility response indicates Mrs. Everywoman's insurance plan covers 100% of cost of semi-private accommodation for two nights' accommodation for post-partum hospital stay. The additional charges for a private room above the semi-private cost, will be invoiced to the patient.
Each Friday Dr. Rhino performs tonsillectomies at the Good Health Hospital. Following their surgery his patients remain in hospital for one night. Unless requested, the patients are accommodated in a wardroom.
Patients with extended medical benefits may request semi private and private accommodation. Dr. Rhino's administrator submits eligibility queries to the insurer for all patients with the same insurer.
Each Insurer queried returns an eligibility response showing the type of accommodation coverage eligible for each patient, and the extent to which their plan covers the accommodation.
|
||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of application roles and their relationships in the Version 3 Guide.
An application responsible for requesting information from public or private healthcare insurers concerning whether a person's insurance coverage is in effect.
This request is for validating whether the patient's insurance policy (coverage) is in effect for a specified date.
The response to this query may impact which products or services will be rendered to the patient and who will pay for them.
An application responsible for requesting information from public or private healthcare insurers concerning whether a person's insurance coverage is in effect for chiro physio benefits coverage.
The request is for validating whether the patient's insurance policy (coverage) is in effect for a specified date).
An application responsible for requesting information from public or private healthcare insurers concerning whether a person's insurance coverage is in effect for generic benefits coverage.
The request is for validating whether the patient's insurance policy (coverage) is in effect for a specified date.
The response to this query may impact which products or services will be rendered to the patient and who will pay for them.
An application responsible for requesting information from public or private healthcare insurers concerning whether a person's insurance coverage is in effect for hospital benefits coverage.
The request is for validating whether the patient's insurance policy (coverage) is in effect for a specified date.
The response to this query may impact which products or services will be rendered to the patient and who will pay for them.
An application responsible for requesting information from public or private healthcare insurers concerning whether a person's insurance coverage is in effect for pharmacy benefits coverage.
The request is for validating whether the patient's insurance policy (coverage) is in effect for a specified date.
The response to this query may impact which products or services will be rendered to the patient and who will pay for them.
An application responsible for requesting information from public or private healthcare insurers concerning whether a person's insurance coverage is in effect for physician benefits coverage.
The request is for validating whether the patient's insurance policy (coverage) is in effect for a specified date).
An application responsible for requesting information from public or private healthcare insurers concerning whether a person's insurance coverage is in effect for preferred accommodation benefits coverage.
The request is for validating whether the patient's insurance policy (coverage) is in effect for a specified date).
The response to this query may impact what accommodation types are available to the patient and who will pay for them.
An application that provides information about whether a patient's healthcare insurance coverage is in effect for a specified date.
Typical responses for an Eligibility Request are Yes, the patient's insurance policy is in effect on the specified date or No, the patient does not have insurance coverage on the specified date.
This response does not necessarily imply that a specific service or product will be covered for payment. It simply informs the Eligibility Requestor (Provider) that the patient has coverage and is qualified to receive benefits on a specified date. An Authorization Request or Pre-Determination Invoice must be submitted if a Provider is seeking commitment from the Authorization Manager (Payor) for payment of a specific service or product.
The Eligibility Requestor (Provider) may use Eligibility Results to determine what services to render and how to collect payment for services.
An application that provides information about whether a patient's healthcare insurance coverage is in effect for a specified date.
Typical responses for an Eligibility Request are Yes, the patient's insurance policy is in effect on the specified date or No, the patient does not have insurance coverage on the specified date.
This response does not necessarily imply that a specific service or product will be covered for payment. It simply informs the Eligibility Requestor (Provider) that the patient has coverage and is qualified to receive benefits on a specified date. An Authorization Request or Pre-Determination Invoice must be submitted if a Provider is seeking commitment from the Authorization Manager (Payor) for payment of a specific service or product.
The Eligibility Requestor (Provider) may use Eligibility Results to determine what services to render and how to collect payment for services.
An application that provides information about whether a patient's healthcare insurance coverage is in effect for a specified date.
Typical responses for an Eligibility Request are Yes, the patient's insurance policy is in effect on the specified date or No, the patient does not have insurance coverage on the specified date.
This response does not necessarily imply that a specific service or product will be covered for payment. It simply informs the Eligibility Requestor (Provider) that the patient has coverage and is qualified to receive benefits on a specified date. An Authorization Request or Pre-Determination Invoice must be submitted if a Provider is seeking commitment from the Authorization Manager (Payor) for payment of a specific service or product.
The Eligibility Requestor (Provider) may use Eligibility Results to determine what services to render and how to collect payment for services.
An application that provides information about whether a patient's healthcare insurance coverage is in effect for a specified date.
Typical responses for an Eligibility Request are Yes, the patient's insurance policy is in effect on the specified date or No, the patient does not have insurance coverage on the specified date.
This response does not necessarily imply that a specific service or product will be covered for payment. It simply informs the Eligibility Requestor (Provider) that the patient has coverage and is qualified to receive benefits on a specified date. An Authorization Request or Pre-Determination Invoice must be submitted if a Provider is seeking commitment from the Authorization Manager (Payor) for payment of a specific service or product.
The Eligibility Requestor (Provider) may use Eligibility Results to determine what services to render and how to collect payment for services.
An application that provides information about whether a patient's healthcare insurance coverage is in effect for a specified date.
Typical responses for an Eligibility Request are Yes, the patient's insurance policy is in effect on the specified date or No, the patient does not have insurance coverage on the specified date.
This response does not necessarily imply that a specific service or product will be covered for payment. It simply informs the Eligibility Requestor (Provider) that the patient has coverage and is qualified to receive benefits on a specified date. An Authorization Request or Pre-Determination Invoice must be submitted if a Provider is seeking commitment from the Authorization Manager (Payor) for payment of a specific service or product.
The Eligibility Requestor (Provider) may use Eligibility Results to determine what services to render and how to collect payment for services.
An application that provides information about whether a patient's healthcare insurance coverage is in effect for a specified date.
Typical responses for an Eligibility Request are Yes, the patient's insurance policy is in effect on the specified date or No, the patient does not have insurance coverage on the specified date.
This response does not necessarily imply that a specific service or product will be covered for payment. It simply informs the Eligibility Requestor (Provider) that the patient has coverage and is qualified to receive benefits on a specified date. An Authorization Request or Pre-Determination Invoice must be submitted if a Provider is seeking commitment from the Authorization Manager (Payor) for payment of a specific service or product.
The Eligibility Requestor (Provider) may use Eligibility Results to determine what services to render and how to collect payment for services.
An application that provides information about whether a patient's healthcare insurance coverage is in effect for a specified date.
Typical responses for an Eligibility Request are Yes, the patient's insurance policy is in effect on the specified date or No, the patient does not have insurance coverage on the specified date.
This response does not necessarily imply that a specific service or product will be covered for payment. It simply informs the Eligibility Requestor (Provider) that the patient has coverage and is qualified to receive benefits on a specified date. An Authorization Request or Pre-Determination Invoice must be submitted if a Provider is seeking commitment from the Authorization Manager (Payor) for payment of a specific service or product.
The Eligibility Requestor (Provider) may use Eligibility Results to determine what services to render and how to collect payment for services.
|
||||||||
|
For details on the interpretation of this section, see the discussion of trigger events in the Version 3 Guide.
| Type: | User request |
A trigger to send an Eligibility Request to determine eligibility for coverage.
This request is for validating whether a patient has healthcare benefits coverage in effect for a specified date, with or without the specification of a particular insurance policy (coverage) in effect for a specified date.
| Type: | Interaction based |
A trigger to send an Eligilbity Query Response message, indicating a patient's eligiblity for healthcare insurance coverage.
Typical responses are Yes: the patient's insurance policy is in effect on the specified date or No: the patient does not have insurance coverage on the specified date.
This response does not necessarily imply that a specific service or product will be covered for payment. It simply informs the Provider that the patient has coverage and is qualified to receive benefits. An Authorization Request or Pre-Determination Request must be submitted if a Provider is trying to determine if a specific service and/or product is covered by the patient's coverage.
|
||||||||
|
For details on the interpretation of this section, see the description of RMIMs in the Version 3 Guide.
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
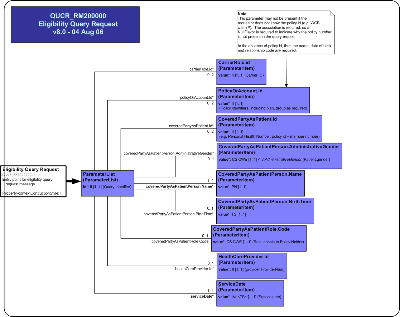
This model represents a message used to send a request for eligilbity for benefit coverage from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
Prior to performing a billable act and invoicing, the Provider may attempt to determine eligibility for coverage for a specified patient (Covered Party). This is a simple verification to determine if the Insurance Carrier/Adjudicator is aware of the patient and that a specific insurance policy is in effect on a particular date.
The query has a number of parameters (e.g. patient name, birth date, carrier id, policy id and date of service) used to form the question.
| Eligibility Query Request | QUCR_HD200100UV01 |
| Eligibility Query Request Hospital | QUCR_HD200800UV03 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
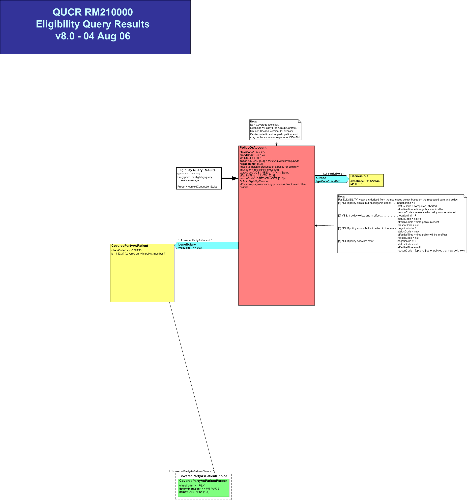
This model represents a message used to respond to a request for eligilbity for benefit coverage made by a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
The eligibility results are a simple Yes/No response, with additional information if the answer is No.
It is important to note that a response of Yes does not imply that an Insurance Carrier/Adjudicator will pay for any Invoice subsequently submitted for that patient on the date of service specified with the query request. Providers are encouraged to use the Authorization Request, COverage Extension Request and/or Pre-Determination Request messages prior to delivery of services and/or goods if they want assurance of payment.
| Eligibility Query Results | QUCR_HD210100UV01 |
| Eligibility Query Results Hospital | QUCR_HD210800UV03 |
|
||||||||||||
|
For details on the interpretation of this section, see the description of HMDs in the Version 3 Guide.
This message is a Query Eligibility submission request to a Provider for information as to whether a Patient has coverage with a Payor as of a given date (Date of Service).
The query is a set of parameters (e.g. Patient id, name, birth date, relationship to Policy Holder and the Carrier id, policy id and date of service). These identify the Covered Party, their insurance and the date of service.
This message returns a negation indicator which is used to indicate presence of a policy. Thus along with an "active" status confirms eligibility (that the Patient has insurance coverage on the requested date). Specific reason codes may also be returned to provide additional clarification about the policy status such as why the policy was terminated. This response to the query is always immediate (i.e. no polling of responses).
It is important to note that an Eligible Response does not imply that a Payor will pay for any Invoice subsequently submitted for that Patient on the Date of Service. Providers are encouraged to use Authorization Request, Coverage Extension Request and Pre-Determination Request messages prior to delivery of services if they want greater assurance of payment.
This message is a Query Eligibility submission request to a Provider for information as to whether a Patient has coverage with a Payor as of a given date (Date of Service).
The query is a set of parameters (e.g. Patient id, name, birth date, relationship to Policy Holder and the Carrier id, policy id and date of service). These identify the Covered Party, their insurance and the date of service.
This message returns a negation indicator which is used to indicate presence of a policy. Thus along with an "active" status confirms eligibility (that the Patient has insurance coverage on the requested date). Specific reason codes may also be returned to provide additional clarification about the policy status such as why the policy was terminated. This response to the query is always immediate (i.e. no polling of responses).
It is important to note that an Eligible Response does not imply that a Payor will pay for any Invoice subsequently submitted for that Patient on the Date of Service. Providers are encouraged to use Authorization Request, Coverage Extension Request and Pre-Determination Request messages prior to delivery of services if they want greater assurance of payment.
This message is a response to a Query Eligibility Request submission. It provides the Provider with information as to whether a Patient has coverage with a Payor as of a given date (Date of Service). This message returns a negation indicator which is used to indicate presence of a policy. Thus along with an "active" status confirms eligibility (that the Patient has insurance coverage on the requested date). Specific reason codes may also be returned to provide additional clarification about the policy status such as why the policy was terminated. This response to the query is always immediate (i.e. no polling of responses).
It is important to note that an Eligible Response does not imply that a Payor will pay for any Invoice subsequently submitted for that Patient on the Date of Service. Providers are encouraged to use Authorization Request, Coverage Extension Request and Pre-Determination Request messages prior to delivery of services if they want greater assurance of payment.
This message is a response to a Query Eligibility Request submission. It provides the Provider with information as to whether a Patient has coverage with a Payor as of a given date (Date of Service). This message returns a negation indicator which is used to indicate presence of a policy. Thus along with an "active" status confirms eligibility (that the Patient has insurance coverage on the requested date). Specific reason codes may also be returned to provide additional clarification about the policy status such as why the policy was terminated. This response to the query is always immediate (i.e. no polling of responses).
It is important to note that an Eligible Response does not imply that a Payor will pay for any Invoice subsequently submitted for that Patient on the Date of Service. Providers are encouraged to use Authorization Request, Coverage Extension Request and Pre-Determination Request messages prior to delivery of services if they want greater assurance of payment.
|
||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the definition of Interactions in the Version 3 Guide.
The sender sends an Eligibility Query Request message to request the status of a patient's eligibility for Chiro Physio services.
| Trigger Event | Eligibility Query Request | QUCR_TE200101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Eligibility Event Query Request Generic | QUCR_MT200101UV01 |
| Reason | Trigger Event | Interaction |
| Eligibility Query Response | QUCR_TE210101UV01 | QUCR_IN210104UV02 |
| Sender | Elig Rqstr, ChiroPhysio | FICR_AR021004UV02 |
| Receiver | Elig Query Mgr, ChiroPhysio | FICR_AR022004UV02 |
The sender sends an Eligibility Query Request message to request the status of a patient's eligibility for Generic services.
| Trigger Event | Eligibility Query Request | QUCR_TE200101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Eligibility Event Query Request Generic | QUCR_MT200101UV01 |
| Reason | Trigger Event | Interaction |
| Eligibility Query Response | QUCR_TE210101UV01 | QUCR_IN210101UV01 |
| Sender | Elig Rqstr, Gen | FICR_AR021001UV01 |
| Receiver | Elig Query Mgr, Gen | FICR_AR022001UV01 |
The sender sends an Eligibility Query Request message to request the status of a patient's eligibility for Hospital services.
| Trigger Event | Eligibility Query Request | QUCR_TE200101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Eligibility Event Query Request Hospital | QUCR_MT200802UV03 |
| Reason | Trigger Event | Interaction |
| Eligibility Query Response | QUCR_TE210101UV01 | QUCR_IN210108UV03 |
| Sender | Elig Rqstr, Hospital | FICR_AR021008UV03 |
| Receiver | Elig Query Mgr, Hospital | FICR_AR022008UV03 |
The sender sends an Eligibility Query Request message to request the status of a patient's eligibility for Pharmacy services.
| Trigger Event | Eligibility Query Request | QUCR_TE200101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Eligibility Event Query Request Generic | QUCR_MT200101UV01 |
| Reason | Trigger Event | Interaction |
| Eligibility Query Response | QUCR_TE210101UV01 | QUCR_IN210102UV01 |
| Sender | Elig Rqstr, Rx | FICR_AR021002UV01 |
| Receiver | Elig Query Mgr, Rx | FICR_AR022002UV01 |
The sender sends an Eligibility Query Request message to request the status of a patient's eligibility for Physician services.
| Trigger Event | Eligibility Query Request | QUCR_TE200101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Eligibility Event Query Request Generic | QUCR_MT200101UV01 |
| Reason | Trigger Event | Interaction |
| Eligibility Query Response | QUCR_TE210101UV01 | QUCR_IN210107UV01 |
| Sender | Elig Rqstr, Physician | FICR_AR021007UV03 |
| Receiver | Elig Query Mgr, Physician | FICR_AR022007UV03 |
The sender sends an Eligibility Query Request message to request the status of a patient's eligibility for Preferred Accommodation services.
| Trigger Event | Eligibility Query Request | QUCR_TE200101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Eligibility Event Query Request Generic | QUCR_MT200101UV01 |
| Reason | Trigger Event | Interaction |
| Eligibility Query Response | QUCR_TE210101UV01 | QUCR_IN210103UV01 |
| Sender | Elig Rqstr, PAccom | FICR_AR021003UV01 |
| Receiver | Elig Query Mgr, PAccom | FICR_AR022003UV01 |
The sender sends an Eligibility Query Response message, which provides information about a patient's eligibility for Chiro Physio services.
The response of this interaction does not necessarily imply a specific service or product will be covered for payment.
| Trigger Event | Eligibility Query Response | QUCR_TE210101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Eligibility Event Query Results Generic | QUCR_MT210101UV01 |
| Sender | Elig Query Mgr, ChiroPhysio | FICR_AR022004UV02 |
| Receiver | Elig Rqstr, ChiroPhysio | FICR_AR021004UV02 |
The sender sends an Eligibility Query Response message, which provides information about a patient's eligibility for Generic services.
The response of this interaction does not necessarily imply a specific service or product will be covered for payment.
| Trigger Event | Eligibility Query Response | QUCR_TE210101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Eligibility Event Query Results Generic | QUCR_MT210101UV01 |
| Sender | Elig Query Mgr, Gen | FICR_AR022001UV01 |
| Receiver | Elig Rqstr, Gen | FICR_AR021001UV01 |
The sender sends an Eligibility Query Response message, which provides information about a patient's eligibility for Hospital services.
The response of this interaction does not necessarily imply a specific service or product will be covered for payment.
| Trigger Event | Eligibility Query Response | QUCR_TE210101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Eligibility Event Query Results Hospital | QUCR_MT210802UV03 |
| Sender | Elig Query Mgr, Hospital | FICR_AR022008UV03 |
| Receiver | Elig Rqstr, Hospital | FICR_AR021008UV03 |
The sender sends an Eligibility Query Response message, which provides information about a patient's eligibility for Pharmacy services.
The response of this interaction does not necessarily imply a specific service or product will be covered for payment.
| Trigger Event | Eligibility Query Response | QUCR_TE210101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Eligibility Event Query Results Generic | QUCR_MT210101UV01 |
| Sender | Elig Query Mgr, Rx | FICR_AR022002UV01 |
| Receiver | Elig Rqstr, Rx | FICR_AR021002UV01 |
The sender sends an Eligibility Query Response message, which provides information about a patient's eligibility for Physician services.
The response of this interaction does not necessarily imply a specific service or product will be covered for payment.
| Trigger Event | Eligibility Query Response | QUCR_TE210101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Eligibility Event Query Results Generic | QUCR_MT210101UV01 |
| Sender | Elig Query Mgr, Physician | FICR_AR022007UV03 |
| Receiver | Elig Rqstr, Physician | FICR_AR021007UV03 |
The sender sends an Eligibility Query Response message, which provides information about a patient's eligibility for Preferred Accommodation services.
The response of this interaction does not necessarily imply a specific service or product will be covered for payment.
| Trigger Event | Eligibility Query Response | QUCR_TE210101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Eligibility Event Query Results Generic | QUCR_MT210101UV01 |
| Sender | Elig Query Mgr, PAccom | FICR_AR022003UV01 |
| Receiver | Elig Rqstr, PAccom | FICR_AR021003UV01 |
| Return to top of page |

