 ANSI/HL7 V3 CR, R4-2008 HL7 Version 3 Standard: Claims and Reimbursement, Release 4 02/20/2008 |
Content Last Edited: 2009-09-04T22:38:52
4.2 Storyboards
4.3 Application Roles
4.4 Trigger Events
4.5 Refined Message Information Models
4.6 Hierarchical Message Descriptions
4.7 Interactions
Coverage extension, or special authorization, provides a mechanism for a Provider to request inclusion of a service and/or product as a covered benefit under a patient's insurance policy. Typically, the service and/or product is not covered under the patient's insurance and a coverage extension request is required before the service and/or product can be paid.
A coverage extension number may also be supplied with the coverage extension results and may be required for inclusion in an Invoice.
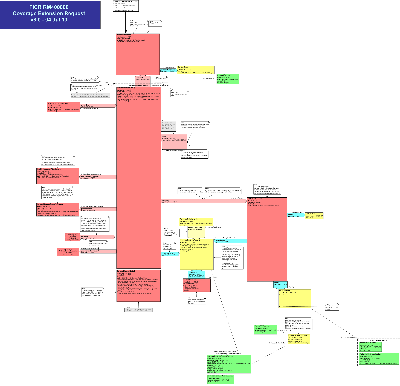
State Transition Diagram
|
||||||||
|
For details on the interpretation of this section, see the storyboard discussion in the Version 3 Guide.
To demonstrate how Coverage Extension for Pharmacy services is requested and obtained. A Coverage Extension by a Coverage Extension Manager is a commitment to extend coverage for a particular insurance policy.
| Cov Ext Request, Rx | |
| Cov Ext Comp Results, Comp, Rx |
Adam Everyman suffers from arthritis and is not responding to his current medication. During a follow-up visit to his physician, Dr. Family, he mentions that his current medication doesn't seem to be working.
Dr. Family suggests Celebrex as an alternative. Celebrex is not a benefit under Adam's health insurance plan, but it may be covered if he applies for and is approved through Coverage Extension.
Dr. Family submits a Coverage Extension request to Adam's insurance company for processing. Results and final approval were sent by the insurance company indicating that the Coverage Extension would be valid for one year.
Dr. Family then provides Adam with a new prescription for Celebrex, which he takes to his local pharmacy to be filled. At the pharmacy, Adam's pharmacist submits a bill to his insurance company for the Celebrex as well as the pharmacist's professional service fee.
Eve Everywoman suffers from Osteoporosis and has been taken her current medication for about one year. During a follow-up visit to her physician, Dr. Family, she undergoes a bone mineral density (BMD) test. Her T-score indicates that her BMD has not increased.
Dr. Family suggests Fosomax as an alternative to her current medication. Fosomax is not an eligible benefit under Eve's health insurance plan, but it may be covered if she applies for and is approved through Coverage Extension.
Dr. Family submits a Coverage Extension request to Eve's insurance company for processing. Eve's insurance company accepted and approved the request and indicates that the authorization is valid for two years.
Dr. Family then provides Eve with a new prescription for Fosomax which she takes to her local pharmacy to be filled. At the pharmacy, Eve's pharmacist submits a bill to her insurance company for the Fosomax as well as the pharmacist's professional service fee.
To demonstrate how Coverage Extension for Pharmacy services is requested and obtained. A Coverage Extension by a Coverage Extension Manager is a commitment to extend coverage for a particular insurance policy.
This storyboard depicts a delayed response with an initial 'identifier handshake' response followed by final Coverage Extension results.
| Cov Ext Request, Init/Comp, Rx | |
| Cov Ext Init Results, Init/Comp, Rx | |
| Cov Ext Comp Results, Init/Comp, Rx |
Eve Everywoman suffers from Osteoporosis and has been taking her current medication for about one year. During a follow-up visit to her physician, Dr. Family, she undergoes a bone mineral density (BMD) test. Her T-score indicates that her BMD has not increased.
Dr. Family suggests Fosomax as an alternative to her current medication. Fosomax is not an eligible benefit under Eve's health insurance plan, but it may be covered if she applies for and is approved through Coverage Extension.
Dr. Family submits an authorization request to Eve's insurance company for processing. Eve's insurance company accepted the Coverage Extension request and sent Dr. Family preprocessing results, which stated that manual processing was required and final results would follow. Two days later, approval for the Coverage Extenstion Request was received. Authorization would be valid for two years.
Dr. Family then provided Eve with a new prescription for Fosomax, which she took to her local pharmacy to be filled. At the pharmacy, Eve's pharmacist submited a bill to her insurance company for the Fosomax as well as the pharmacist's professional service fee.
|
||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of application roles and their relationships in the Version 3 Guide.
An application that requests approval to extend a patient's coverage benefits for delivery of healthcare services (e.g. treatment, diagnosis) and/or products (e.g. wheelchair, hearing aid), typically before the services and/or products have been rendered.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Coverage Extension Requests that are approved typically have expiration dates and limits on their use.
The Coverage Extension Requestor will receive only the Final Coverage Extension Results with no initial response from the Coverage Extension Manager.
An application that requests approval to extend a patient's coverage benefits for delivery of pharmaceutical services (e.g. glucometer training, home visit) and/or products (e.g. medication, blood pressure monitor), typically before the services and/or products have been rendered.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Coverage Extension Requests that are approved typically have expiration dates and limits on their use.
The Coverage Extension Requestor will receive only the Final Coverage Extension Results with no initial response from the Coverage Extension Manager.
An application that requests approval to extend a patient's coverage benefits for delivery of healthcare services (e.g. treatment, diagnosis) and/or products (e.g. wheelchair, hearing aid), typically before the services and/or products have been rendered.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Coverage Extension Requests that are approved typically have expiration dates and limits on their use.
The Coverage Extension Requestor will receive only the Final Coverage Extension Results with no initial response from the Coverage Extension Manager.
An application that requests approval to extend a patient's coverage benefits for delivery of healthcare services (e.g. treatment, diagnosis) and/or products (e.g. wheelchair, hearing aid), typically before the services and/or products have been rendered.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Coverage Extension Requests that are approved typically have expiration dates and limits on their use.
The Coverage Extension Requestor will receive an initial response, which may contain partial results and an indication when the final Coverage Extension Results will be forwarded from the Coverage Extension Manager.
An application that requests approval to extend a patient's coverage benefits for pharmaceutical services (e.g. glucometer training, home visit) and/or products (e.g. medication, blood pressure monitor), typically before the services and/or products have been rendered.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Coverage Extension Requests that are approved typically have expiration dates and limits on their use.
The Coverage Extension Requestor will receive an initial response, which may contain partial results and an indication when the final Coverage Extension Results will be forwarded from the Coverage Extension Manager.
An application that requests approval to extend a patient's coverage benefits for delivery of healthcare services (e.g. treatment, diagnosis) and/or products (e.g. wheelchair, hearing aid), typically before the services and/or products have been rendered.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Coverage Extension Requests that are approved typically have expiration dates and limits on their use.
The Coverage Extension Requestor will receive an initial response, which may contain partial results and an indication when the final Coverage Extension Results will be forwarded from the Coverage Extension Manager.
An application that responds to a Coverage Extension Request, Generic with the Final Coverage Extension Results only.
The Final Coverage Extension Results may grant or deny Coverage Extension for a generic benefits group to render healthcare services or supply products. If the Coverage Extension is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Coverage Extension is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
The Final Coverage Extension Results to a Coverage Extension Request may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Coverage Extension Request by a period of time (perhaps one or more days).
An application that responds to a Coverage Extension Request, Pharmacy with the Final Coverage Extension Results only.
The Final Coverage Extension Results may grant or deny Coverage Extension for rendering pharmaceutical services or products. If the Coverage Extension is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Coverage Extension is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
The Final Coverage Extension Results to a Coverage Extension Request may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Coverage Extension Request by a period of time (perhaps one or more days).
An application that responds to a Coverage Extension Request with the Final Coverage Extension Results only.
The Final Coverage Extension Results may grant or deny Coverage Extension for rendering healthcare services or supplying products. If the Coverage Extension is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Coverage Extension is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
The Final Coverage Extension Results to a Coverage Extension Request may arrive close to immediate (i.e. in the same query/response interaction) or may lag the Coverage Extension Request by a period of time (perhaps one or more days).
An application that responds to a Coverage Extension Request, Generic with Final Coverage Extension Results if possible. If Final Coverage Extension Results are not possible, then the Coverage Extension Manager may respond with Initial Coverage Extension Results that can include partial or incomplete processing results and an indication of when the Final Coverage Extension Results will be available.
When the Coverage Extension Manager, Initial/Final Results sends the completed Coverage Extension Results, they act as a Coverage Extension Notifier. This Application Role includes the Notifier Application Role.
The Final Coverage Extension Results may grant or deny Coverage Extension to a generic benefits group for rendering healthcare services or supplying products. If the Coverage Extension is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Coverage Extension is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
An application that responds to a Coverage Extension Request, Pharmacy with Final Coverage Extension Results if possible. If Final Coverage Extension Results are not possible, then the Coverage Extension Manager may respond with Initial Coverage Extension Results that can include partial or incomplete processing results and an indication of when the Final Coverage Extension Results will be available.
When the Coverage Extension Manager, Initial/Final Results sends the completed Coverage Extension Results, they act as a Coverage Extension Notifier. This Application Role includes the Notifier Application Role.
The Final Coverage Extension Results may grant or deny Coverage Extension for rendering pharmaceutical services or supplying pharmaceutical products. If the Coverage Extension is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product.
An application that responds to a Coverage Extension Request with Final Coverage Extension Results if possible. If Final Coverage Extension Results are not possible, then the Coverage Extension Manager may respond with Initial Coverage Extension Results that can include partial or incomplete processing results and an indication of when the Final Coverage Extension Results will be available.
When the Coverage Extension Manager, Initial/Final Results sends the completed Coverage Extension Results, they act as a Coverage Extension Notifier. This Application Role includes the Notifier Application Role.
The Final Coverage Extension Results may grant or deny Coverage Extension for rendering healthcare services or supplying products. If the Coverage Extension is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product.
An application responsible for sending notification of Final Authorization Results to an Authorization Tracker.
An application responsible for sending notification of Final Authorization Results, Generic to an Authorization Tracker.
An application responsible for sending notification of Final Authorization Results, Pharmacy to an Authorization Tracker.
An application responsible for tracking Authorization Results from an Authorization Notifier.
An example of a Coverage Extension Tracker could be a head office, accountant or a payee.
An application responsible for tracking Authorization Results, Generic from an Authorization Notifier.
An example of a Coverage Extension Tracker could be a head office, accountant or a payee.
An application responsible for tracking Authorization Results, Pharmacy from an Authorization Notifier.
An example of a Coverage Extension Tracker could be a head office, accountant or a payee.
|
||||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of trigger events in the Version 3 Guide.
| Type: | State-transition based |
| State Transition: | PaymentRequest (FICR_RM400000UV01) |
A trigger to send a Coverage Extenstion for extending a patient's coverage for additional services (e.g., treatment, drug) and/or products (e.g., wheelchair, hearing aid); typically before the services and/or products have been rendered.
An approved Coverage Extension Request does NOT represent an Adjudicators commitment to pay for a service and/or product.
The Provider may or may not actually bill for the service and/or product that is added to a patient's coverage.
| Type: | Interaction based |
A trigger to send an initial Coverage Extension Results when the Adjudicator has completed an initial preprocessing of the Coverage Extension Request.
This trigger occurs in the same query/response interaction as the Coverage Extension Request; and will subsequently be followed by a trigger to the Coverage Extension Manager, Final, when the Final Results are complete.
The Initial Results may include preliminary edits such as patient identifier and date validation as well as patient eligibility validation. The Initial Results will also indicate when the Final Coverage Extention Results may be expected.
The Final Coverage Extension Results may grant or deny Coverage Extension for rendering healthcare services or supplying products. If Coverage Extension is denied, the Adjudicator will not pay for any costs incurred in the delivery of the specified service or product. If the Coverage Extension is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
| Type: | State-transition based |
| State Transition: | PaymentIntent (FICR_RM410000UV01) |
A trigger to send a completed Coverage Extension Result.
This trigger may be fired close to immediate (i.e., in the same submission/response interaction as the request) or may lag the request by a period of time (perhaps one or more days).
The completed Coverage Extension Results may grant or deny coverage extension for services and/or products. If Coverage Extension is denied, the Adjudicator will not pay for any costs incurred in the delivery of the specified service and/or product. If the Coverage Extension is granted, the maximum amount that will be paid for the service and/or product may be included in the response.
Approved Coverage Extensions do NOT represent a commitment to pay for the service and/or product by the Adjudicator.
| Type: |
A trigger that indicated that the Adjudicator has accepted responsibility for the Coverage Extension Nullify Request and will respond with completed results (accept, reject) at a later point (e.g. next day).
| Type: |
A trigger that indicated successful completion of a Coverage Extension Nullify Request. In other words, the request has been nullified.
| Type: | State-transition based |
| State Transition: | InvoiceElementGroup (FICR_RM420000UV01) |
A trigger to send a Coverage Extension Nullify Request.
The response to the request may be accepted or rejected, depending on the ability of the Adjudicator to nullify the request.
| Type: |
A trigger that indicated unsuccessful completion of a Coverage Extension Nullify Request. In other words, the request has NOT been nullified.
| Type: | Interaction based |
A trigger to send a Coverage Extension Query Response indicating the existence and status of a Coverage Extension Request.
Coverage Extension Query Response may indicate that the Coverage Extension Request processing is not completed; or if completed, will confirm that Coverage Extension was given or will indicate that Coverage Extension was denied.
|
||||||||||||
|
For details on the interpretation of this section, see the description of RMIMs in the Version 3 Guide.
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to submit a Coverage Extension Request from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
It is to obtain extension of the insurance coverage to include the specified services or supply of specified products. This is required when the products or services are not normally covered. Only in certain circumstances that are specified and confirmed by the practitioner, will the items be covered. The coverage may be specified more generically than in an authorization. Quantities and costing are optional in the request.
The core class referenced in the RMIM is the InvoiceElement, cloned as the InvoiceElementOrderGroup and InvoiceElementOrderDetail.
The message structure is the same as the Authorization Request including specification of the subject, PolicyOrAccount (insurance), FinancialContract, HealthDocumentAttachment and A_Billable act.
| Coverage Extension Request Generic | FICR_HD400100UV01 |
| Coverage Extension Request Pharmacy | FICR_HD400200UV01 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to respond to a request for Coverage Extension from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
It is the result of a request for insurance coverage extension for specified services or products.
The coverage extension response will specify approval/denial of the extension and possibly limits to the coverage. These are specified as AdjudicationResultsInformation item (OBS: observations) values as pertinent information to the AdjudicationResult.
The core classes referenced in the RMIM are the InvoiceElement, cloned as the InvoiceElementOrderGroup and InvoiceElementOrderDetail. These specify the items that coverage will be extended to and the billable act may provide further clinical details.
The message structure is the same as the Authorization Results without all of the details.
| Coverage Extension Results Generic | FICR_HD410100UV01 |
| Coverage Extension Results Pharmacy | FICR_HD410200UV01 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to Nullify a previous Coverage Extension Request from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
The core class referenced in the RMIM is the InvoiceElement, cloned as the InvoiceElementOrderGroup.The message references one group in the Coverage Extension request.
| Coverage Extension Nullify Request | FICR_HD420100UV01 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to send the Coverage Extension Query Request message from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
It is a query on the status of a previous Coverage Extension Request.
The query is a single parameter, the Invoice Element root Group identifier, from the Coverage Extension Request being queried.
The Coverage Extension Results message is returned in response to this query.
| Coverage Extension Query Request | QUCR_HD440100UV01 |
|
||||||||||||||||
|
For details on the interpretation of this section, see the description of HMDs in the Version 3 Guide.
This message is used to send results of a generic Coverage Extension Request to a Provider Application. If the extension is approved, then the Adjudicator Application may return either an Authorization Number (AdjudicatedElementGroup identifier) or an individual who is the responsible entity authorizing the items. The extension status and limitations are specified as AdjudicationResultsInformation observation values.
This message is used to send results of a Pharmacy Coverage Extension Request to a Provider Application. If the extension is approved, then the Adjudicator Application may return either an Authorization Number (AdjudicatedElementGroup identifier) or an individual who is the responsible entity authorizing the items. The extension status and limitations are specified as AdjudicationResultsInformation observation values.
This message is used to Nullify a Coverage Extension Request previously submitted.
This message can be used to Nullify an individual Invoice Element Group within a request.
This message cannot be used to update ancillary information in a Coverage Extension Request that has been submitted. The original request must be Nullified, and a new Coverage Extension Request submitted to the Adjudicator.
This message requests the status of a Coverage Extension Request.
The query is a single parameter, the Invoice Element root Group identifier, from the Coverage Extension Request being queried.
The Coverage Extension Results message is returned in response to this query.
|
||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the definition of Interactions in the Version 3 Guide.
The sender sends a Coverage Extension Results message containing the inital Coverage Extension Results for Generic services and/or products. Completed results will follow at a later point in time (e.g. next day).
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Complete Initial Confirmation | FICR_TE410102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Complete Generic | FICR_MT410101UV01 |
| Sender | Cov Ext Mgr, Initial/Fnl Rslts, Gen | FICR_AR043001UV01 |
| Receiver | Cov Ext Rqstr, Init/Comp Rslts, Gen | FICR_AR041001UV01 |
The sender sends a Coverage Extension Results message containing the inital Coverage Extension Results for Pharmacy services and/or products. Completed results will follow at a later point in time (e.g. next day).
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Complete Initial Confirmation | FICR_TE410102UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Complete Pharmacy | FICR_MT410201UV01 |
| Sender | Cov Ext Mgr, Initial/Fnl Rslts, Rx | FICR_AR043002UV01 |
| Receiver | Cov Ext Rqstr, Init/Comp Rslts, Rx | FICR_AR041002UV01 |
The sender sends a Coverage Extension Request message for Generic services and/or products.
The receiver will provide completed Coverage Extension Results, NOT initial results.
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Request | FICR_TE400101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Activate Generic | FICR_MT400101UV01 |
| Reason | Trigger Event | Interaction |
| Completed Coverage Extension Results | FICR_TE410101UV01 | FICR_IN410101UV01 |
| Sender | Cov Ext Rqstr, Comp Rslts, Gen | FICR_AR040001UV01 |
| Receiver | Cov Ext Mgr, Complete Rslts, Gen | FICR_AR042001UV01 |
The sender sends a Coverage Extension Request message for Pharmacy services and/or products.
The receiver will provide completed Coverage Extension Results, NOT initial results.
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Request | FICR_TE400101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Activate Pharmacy | FICR_MT400201UV01 |
| Reason | Trigger Event | Interaction |
| Completed Coverage Extension Results | FICR_TE410101UV01 | FICR_IN410102UV01 |
| Sender | Cov Ext Rqstr, Comp Rslts, Rx | FICR_AR040002UV01 |
| Receiver | Cov Ext Mgr, Complete Rslts, Rx | FICR_AR042002UV01 |
The sender sends a Coverage Extension Request message for Generic services and/or products.
The receiver will attempt to return completed Coverage Extension Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Request | FICR_TE400101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Activate Generic | FICR_MT400101UV01 |
| Reason | Trigger Event | Interaction |
| Initial Coverage Extension Results | FICR_TE410102UV01 | FICR_IN410201UV01 |
| Completed Coverage Extension Results | FICR_TE410101UV01 | FICR_IN410301UV01 |
| Sender | Cov Ext Rqstr, Init/Comp Rslts, Gen | FICR_AR041001UV01 |
| Receiver | Cov Ext Mgr, Initial/Fnl Rslts, Gen | FICR_AR043001UV01 |
The sender sends a Coverage Extension Request message for Pharmacy services and/or products.
The receiver will attempt to return completed Coverage Extension Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Request | FICR_TE400101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Activate Pharmacy | FICR_MT400201UV01 |
| Reason | Trigger Event | Interaction |
| Initial Coverage Extension Results | FICR_TE410102UV01 | FICR_IN410202UV01 |
| Completed Coverage Extension Results | FICR_TE410101UV01 | FICR_IN410302UV01 |
| Sender | Cov Ext Rqstr, Init/Comp Rslts, Rx | FICR_AR041002UV01 |
| Receiver | Cov Ext Mgr, Initial/Fnl Rslts, Rx | FICR_AR043002UV01 |
The sender sends a Coverage Extension Results message containing the completed results of a Coverage Extension Request for Generic services and/or products.
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Complete Notification | FICR_TE410101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Complete Generic | FICR_MT410101UV01 |
| Sender | Cov Ext Mgr, Complete Rslts, Gen | FICR_AR042001UV01 |
| Receiver | Cov Ext Rqstr, Comp Rslts, Gen | FICR_AR040001UV01 |
The sender sends a Coverage Extension Results message containing the completed results of a coverage Extension Request for Pharmacy services and/or products.
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Complete Notification | FICR_TE410101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Complete Pharmacy | FICR_MT410201UV01 |
| Sender | Cov Ext Mgr, Complete Rslts, Rx | FICR_AR042002UV01 |
| Receiver | Cov Ext Rqstr, Comp Rslts, Rx | FICR_AR040002UV01 |
The sender sends a Coverage Extension Results message containing the completed results of a coverage Extension Request for Generic services and/or products.
This notification follows on initial results sent previously.
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Complete Notification | FICR_TE410101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Complete Generic | FICR_MT410101UV01 |
| Sender | Cov Ext Mgr, Initial/Fnl Rslts, Gen | FICR_AR043001UV01 |
| Receiver | Cov Ext Rqstr, Init/Comp Rslts, Gen | FICR_AR041001UV01 |
The sender sends a Coverage Extension Results message containing the completed results of a coverage Extension Request for Pharmacy services and/or products.
This notification follows on initial results sent previously.
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Complete Notification | FICR_TE410101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Complete Pharmacy | FICR_MT410201UV01 |
| Sender | Cov Ext Mgr, Initial/Fnl Rslts, Rx | FICR_AR043002UV01 |
| Receiver | Cov Ext Rqstr, Init/Comp Rslts, Rx | FICR_AR041002UV01 |
The sender sends a Coverage Extension Nullify Request message to request the nullification of a previously submitted Coverage Extension Request for Generic services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Coverage Extension Request.
| Trigger Event | Coverage Extension Nullify Request | FICR_TE420101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Nullify Request | FICR_MT420101UV01 |
| Sender | Cov Ext Rqstr, Comp Rslts, Gen | FICR_AR040001UV01 |
| Receiver | Cov Ext Mgr, Complete Rslts, Gen | FICR_AR042001UV01 |
The sender sends a Coverage Extension Nullify Request message to request the nullification of a previously submitted Coverage Extension Request for Pharmacy services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Coverage Extension Request.
| Trigger Event | Coverage Extension Nullify Request | FICR_TE420101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Nullify Request | FICR_MT420101UV01 |
| Sender | Cov Ext Rqstr, Comp Rslts, Rx | FICR_AR040002UV01 |
| Receiver | Cov Ext Mgr, Complete Rslts, Rx | FICR_AR042002UV01 |
The sender sends a Coverage Extension Nullify Request message to request the nullification of a previously submitted Coverage Extension Request for Generic services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Coverage Extension Request.
| Trigger Event | Coverage Extension Nullify Request | FICR_TE420101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Nullify Request | FICR_MT420101UV01 |
| Sender | Cov Ext Rqstr, Init/Comp Rslts, Gen | FICR_AR041001UV01 |
| Receiver | Cov Ext Mgr, Initial/Fnl Rslts, Gen | FICR_AR043001UV01 |
The sender sends a Coverage Extension Nullify Request message to request the nullification of a previously submitted Coverage Extension Request for Pharmacy services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Coverage Extension Request.
| Trigger Event | Coverage Extension Nullify Request | FICR_TE420101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Coverage Extension Event Nullify Request | FICR_MT420101UV01 |
| Sender | Cov Ext Rqstr, Init/Comp Rslts, Rx | FICR_AR041002UV01 |
| Receiver | Cov Ext Mgr, Initial/Fnl Rslts, Rx | FICR_AR043002UV01 |
The sender sends a Coverage Extension Query message to determine the status of a previously submitted Coverage Extension Request for Generic services and/or products.
Query response uses the Coverage Extension Results message.
| Trigger Event | Coverage Extension Query Request | QUCR_TE440101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Coverage Extension Event Query Request | QUCR_MT440101UV01 |
| Reason | Trigger Event | Interaction |
| Coverage Extension Query Response | QUCR_TE450101UV01 | QUCR_IN450101UV01 |
| Sender | Cov Ext Rqstr, Comp Rslts, Gen | FICR_AR040001UV01 |
| Receiver | Cov Ext Mgr, Complete Rslts, Gen | FICR_AR042001UV01 |
The sender sends a Coverage Extension Query message to determine the status of a previously submitted Coverage Extension Request for Pharmacy services and/or products.
Query response uses the Coverage Extension Results message.
| Trigger Event | Coverage Extension Query Request | QUCR_TE440101UV01 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Coverage Extension Event Query Request | QUCR_MT440101UV01 |
| Reason | Trigger Event | Interaction |
| Coverage Extension Query Response | QUCR_TE450101UV01 | QUCR_IN450102UV01 |
| Sender | Cov Ext Rqstr, Comp Rslts, Rx | FICR_AR040002UV01 |
| Receiver | Cov Ext Mgr, Complete Rslts, Rx | FICR_AR042002UV01 |
The sender sends a Coverage Extension Results message containing the processing status (e.g. active, completed) and/or results of a Coverage Extension Request for Generic services and/or products.
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Query Response | QUCR_TE450101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Coverage Extension Event Complete Generic | FICR_MT410101UV01 |
| Sender | Cov Ext Mgr, Complete Rslts, Gen | FICR_AR042001UV01 |
| Receiver | Cov Ext Rqstr, Comp Rslts, Gen | FICR_AR040001UV01 |
The sender sends a Coverage Extension Results message containing the processing status (e.g. active, completed) and/or results of a Coverage Extension Request for Pharmacy services and/or products.
Coverage Extension Results indicate whether the service and/or product has been included in a patient's insurance policy.
| Trigger Event | Coverage Extension Query Response | QUCR_TE450101UV01 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Coverage Extension Event Complete Pharmacy | FICR_MT410201UV01 |
| Sender | Cov Ext Mgr, Complete Rslts, Rx | FICR_AR042002UV01 |
| Receiver | Cov Ext Rqstr, Comp Rslts, Rx | FICR_AR040002UV01 |
| Return to top of page |

