 ANSI/HL7 V3 CR, R4-2008 HL7 Version 3 Standard: Claims and Reimbursement, Release 4 02/20/2008 |
Content Last Edited: 2009-09-04T22:38:52
3.2 Storyboards
3.3 Application Roles
3.4 Trigger Events
3.5 Refined Message Information Models
3.6 Hierarchical Message Descriptions
3.7 Interactions
Authorization provides a mechanism whereby an insurance carrier or designate may require a Provider to obtain pre-approval before a particular service and/or product is covered under a specific insurance policy. For example, some complex procedures and complicated treatment plans require pre-approval prior to delivery and/or billing.
Authorization can also be used by a Provider to confirm that a service and/or product will be paid (and to what extent) prior to delivery of that service and/or product.
Authorization results will typically define the maximum benefit allowed under the authorization, including effective dates, dollar limits and frequencies. Authorization results may also indicate if funds have been set aside under the authorization for Invoices against the authorization.
An authorization number may also be supplied with the authorization results and may be required for inclusion in an Invoice.
State Transition Diagram
|
||||||||||||||||||||
|
For details on the interpretation of this section, see the storyboard discussion in the Version 3 Guide.
To demonstrate when and how a Generic Authorization Request is nullified. The Request is sent to the Authorization Manager to Nullify a previously submitted request for Authorization. The initial Authorization Request may or may not have been responded to with Authorization Results. After Nullifylation, the Payor is no longer committed to pay for previously Authorized services.
| Auth Nullify Request, Gen |
Kari Kidd injures her back when she is playing a game with her friends at school. The school calls for an ambulance to take Kari to the hospital. In the hospital, Kari receives 2 x-rays, a full body checkup, and takes five painkillers. The doctor also keeps Kari in the hospital for 3 days of observation.
After the three days, the doctor discharges Kari but would like her to return in one month to have another set of x-rays taken. An Authorization is required for the second set of X-rays.
The doctor submits an Authorization Request to Kari's insurance company. The Authorization is approved and a number is given to the doctor to quote on the Invoice for the x-rays.
After two weeks, Kari and her mother conclude that she has recovered and no longer has symptoms. Her mother informs the doctor that Kari will not be returning for a second set of x-rays. The doctor agrees and contacts Kari's insurance company to cancel the original Authorization Request for the second set of x-rays. The insurance company acknowledges the receipt of the request and cancels the Authorization Request.
To demonstrate when and how a Preferred Accommodation Authorization Request is nullified. The Request is sent to the Authorization Manager to Nullify a previously submitted request for Authorization. The initial Authorization Request may or may not have been responded to with Authorization Results. After Nullifylation, the Payor is no longer committed to pay for previously Authorized services.
| Auth Nullify Request, PAccom |
Mr. Everyman has been suffering unexplained seizures and is admitted to hospital for testing and observation. He insists on private room accommodation.
Mr. Everyman's insurer limits private room coverage to 3 days without Authorization.
The hospital administrator submits an Authorization Request to the insurer for 4 days additional private room accommodation.
The insurer approves the Authorization Request. There is a $50 per day patient deductible for private accommodation.
After 2 days Mr. Everyman, irritated by the invasive testing and hospital amenities, demands to be discharged under his sister's care.
The hospital contacts Mr. Everyman's insurance company to cancel the original Authorization Request for 4 day's accommodation. The insurance company acknowledges the receipt of the request and cancels the Authorization Request.
To demonstrate how a query is submitted to determine the existence and status of a previously submitted Authorization Request. E.g. A diagnostic facility may wish to confirm that the services to be rendered have received Authorization by the Payor. Results will confirm that Authorization was given or will indicate that Authorization was not provided/requested.
| Auth Query Request, Gen |
Mr. Everyman had not heard back from his physical therapist indicating his health benefit plan would cover the cost of a soft knee brace for a two-month period. At his last visit with the physical therapist, she had indicated that she should hear back from the benefit plan within 2 days.
Three days had elapsed so Mr. Everyman phoned the physical therapist office and asked the clerk if they had payment authorization for the soft knee brace.
The clerk reviewed Mr. Everyman's on-line medical file and noted that they had not received the final response from the benefit plan for the soft knee brace payment. The clerk indicated to Mr. Everyman that they had not received a final response yet, but that if he would hold on for a few minutes, she would send an on-line query to the benefit plan to determine the status of the authorization request.
The clerk submits an on-line query to the benefit plan, quoting authorization number and patient name and receives a response indicating the authorization request is in process and has not yet been approved.
The information is relayed to Mr. Everyman who is told that he will be phoned as soon as the authorization is received.
To demonstrate how a query is submitted to determine the existence and status of a previously submitted Preferred Accommodation Authorization Request.
| Auth Query Request, PAccom |
On Tuesday, Good Health Hospital submitted Authorization Requests to HC Payor, Inc. for 10 patients pre-registered for semi-private and private room accommodation the following Monday morning.
On Thursday, the hospital administrator had only received Authorization Results for 4 of these patients. An Authorization Query was submitted to HC Payor, Inc. for the status of the original Authorization Request.
A response was returned to the administrator with details on the status of the Authorization Request:
-
4 patients - authorization approval sent
-
4 patients - authorization approval given and in transit
-
2 patients - authorization pending.
To demonstrate how Authorization for Generic services is requested and obtained. An Authorization by a Payor is a Payor's commitment to pay for services/products even though a Payor may or may not reserve monies for the approved amount.
| Auth Request, Gen | |
| Auth Comp Results Comp, Gen |
Adam Everyman visits his doctor for a routine check up. During the check up, Dr. Family discovers something that requires a specialized test, which is performed at a local diagnostic facility. In order for the test to be performed, the diagnostic facility must have an Authorization on file and a practitioner with specific qualifications (i.e., Dr. Family) must have registered this Authorization.
Dr. Family checks against Mr. Everyman's insurance coverage with HC Payor, Inc. to see if this test is covered (eligibility check). Dr. Family determines that Mr. Everyman does indeed have coverage with this insuror for this type of test.
Dr. Family then proceeds to register an Authorization against Mr. Everyman's insurance policy. HC Payor, Inc. verifies that Dr. Family is indeed capable/allowed to issue this type of Authorization. Authorization is received from HC Payor, Inc. in the form of an Authorization identifier, along with an expiry date and conditions for that Authorization (e.g., dollar limit, deductibles, etc.). Note: Dr. Family can also bill for the office visit.
Mr. Everyman proceeds to the diagnostic facility to have the test performed. The diagnostic facility verifies that there is an Authorization on file with HC Payor, Inc. for the test for Mr. Everyman (query Authorization Request interaction not shown on ladder diagram). They may also get the number from the patient if they have been given this identifier from Dr. Family. However, they will still verify the Authorization is on file and still active. Note: The diagnostic facility can only verify Authorizations and cannot initiate any Authorizations (HC Payor, Inc. rule).
Once the test has been performed, results are passed to Dr. Family. The diagnostic facility then bills HC Payor, Inc. for the test, quoting the Authorization identifier from HC Payor, Inc..
As a result of an injury to the left knee sustained while in-line skating, a person visits their primary care physician (PCP). Following a preliminary examination, the PCP informs the person that he is ordering an MRI of the left knee. The patient's insurance data is on file as a result this visit. As a function of the process of scheduling the MRI, the patient's coverage is reviewed. It is noted that this service must be authorized prior to being performed. A service request authorization is initiated and the service is scheduled pending authorization. Upon receipt of the authorization, the appointment is finalized and the patient notified. If authorization is denied, the appointment is cancelled and the patient notified of the outcome including any reason for denial.
A worker seriously injured their back on the work site and was taken to the nearest hospital emergency department. During admission it was identified that the patient was injured at the work place. The patient's employer submitted an accident and injury form to the worker's health benefit plan identifying the patient information and accident particulars. A claim was established for the accident.
During the patient's hospital stay, they received numerous x-rays, assessments and treatments from the hospital physical therapists and chiropractic doctor as well as assessment by a surgeon. These services were all covered under the agreement with the service Providers and billed and paid for accordingly.
However, the team decided that the best course of treatment for the patient would be back surgery followed by physical therapy treatment and the use of a wheelchair to increase mobility for the first 6 weeks after surgery. As the use of a wheelchair is not covered under the agreement, Authorization for this service needed to be obtained prior to the surgery. The clerk indicated to the patient that they would try to obtain authorization for this service and would let the patient know within the next few days of the result. The clerk prepared an authorization request for this service to submit to the worker's health benefit plan at the end of the day.
A response to the authorization request was received indicating the worker's health plan gave Authorization for the rental of a wheel chair for a 6-week period. An Authorization number was provided in the response that was to be used for billing of these services under the worker's current claim.
The patient's spouse was given a letter from the worker's health benefit plan indicating the medical supplier the wheelchair could be rented from, the benefit plan and claim information, as well as the Authorization number for the rental. They were also given a claim form that they could manually complete for re-imbursement for the rental of the wheelchair. They were also informed that as an alternative, they could sign onto the health benefit plan's web site, to submit the re-imbursement form for rental of the wheelchair.
The surgery was performed and the wheelchair was ordered. The patient's spouse paid for and picked up the wheelchair. The patient's spouse signed onto the health benefit plan web site and submitted the re-imbursement form indicating the patient information, claim number, Authorization number and details of the wheelchair rental.
A worker seriously injured their back on the work site and was taken to the nearest hospital emergency department. During admission it was identified that the patient was injured at the work place. The patient's employer submitted an accident and injury form to the worker's health benefit plan identifying the patient information and accident particulars. A claim was established for the accident.
During the patient's hospital stay, they received numerous x-rays, assessments and treatments from the hospital physical therapists and chiropractic doctor as well as assessment by a surgeon. These services were all covered under the agreement with the service Providers and billed and paid for accordingly.
However, the team decided that the best course of treatment for the patient would be back surgery followed by physical therapy treatment and the use of a wheelchair to increase mobility for the first 6 weeks after surgery. As physical therapy and wheelchair use is not covered under the agreement, Authorization for these services needed to be obtained. The clerk indicated to the patient that they would try to obtain authorization for these services and would let the patient know within the next few days of the result. The clerk prepared an authorization request for these two services to submit to the worker's health benefit plan at the end of the day.
A response to the authorization request was received indicating the worker's health plan gave Authorization for the physical therapy and rental of a wheel chair for a 6-week period. An Authorization number was provided in the response that was to be used for billing of these services under the worker's current claim.
The patient's spouse was given a letter from the worker's health benefit plan indicating the medical supplier the wheelchair could be rented from, the benefit plan and claim information, as well as the Authorization number for the rental. They were also given a claim form that they could manually complete for re-imbursement for the rental of the wheelchair. They were informed that as an alternative, they could sign onto the health benefit plan's web site, to submit the re-imbursement form for rental of the wheelchair.
The surgery was performed and the wheelchair was ordered. The patient's spouse paid for and picked up the wheelchair. When billing for the physical therapy, the therapist billed the worker's health benefit plan for numerous detailed items that were performed, quoting the Authorization number on each item. The patient's spouse signed onto the health benefit plan web site and submitted the re-imbursement form indicating the patient information, claim number, Authorization number and details of the wheelchair rental.
To demonstrate how Authorization for Preferred Accommodation is requested and obtained. An Authorization by a Payor is a Payor's commitment to pay for services/products even though a Payor may or may not reserve monies for the approved amount.
| Auth Comp Results Comp, PAccom |
Eve Everywoman arrives at Good Health Hospital for her pre-operation appointment for pending cosmetic surgery. The post-operation care should last 3 days.
Ms. Everywoman insists on total seclusion and 24 hour security of her accommodation. She submits recommendations and documentation from her psychologist and medical doctor.
The hospital submits the supporting documentation with an Authorization Request to HC Payor, Inc. for Private Room accommodation and round the clock security protection.
The Authorization Adjudicator at HC Payor, Inc. reviews the request and sends written approval to the hospital for a private room for 2 nights and one security officer designated by the insurer for round-the-clock protection. There is a coverage limit on the Authorization of $1000.00 per day.
Mr. Everyman arrives at the hospital for a scheduled admission on Day 1. At the time of admission he requests a Private Room, and provides his insurance information.
Private Room Accommodation is covered under his employer's extended health insurance plan but an Authorization is required.
The hospital administrator submits an Authorization Request to Mr. Everyman's insurance company for private room accommodation. The Authorization is approved. The Authorization results indicate there is a coverage limit of $250.00 per day for private room accommodation.
The hospital private room charge is $350 per day.
Mr. Everyman is discharged after a 3-night stay; he is charged $300.00 for Private Room accommodation on his VISA account.
The hospital submits an invoice to the insurance carrier for $1050.00, quoting the Authorization Number.
To demonstrate how Authorization for Generic healthcare services is requested and obtained. An Authorization by a Payor is a Payor's commitment to pay for services/products even though a Payor may or may not reserve monies for the approved amount.
This storyboard depicts a delayed response with an initial 'identifier handshake' response followed by final authorization results.
| Auth Request, Init/Comp, Gen | |
| Auth Init Results Init/Comp, Gen | |
| Auth Comp Results Init/Comp, Gen |
A worker seriously injured their back on the work site and was taken to the nearest hospital emergency department. During admission it was identified that the patient was injured at the work place. The patient's employer submitted an accident and injury form to the worker's health benefit plan identifying the patient information and accident particulars. A claim was established for the accident.
During the patient's hospital stay, they received numerous x-rays, assessments and treatments from the hospital physical therapists and chiropractic doctor as well as assessment by a surgeon. These services were all covered under the agreement with the service Providers and billed and paid for accordingly.
However, the team decided that the best course of treatment for the patient would be back surgery followed by physical therapy treatment and the use of a wheelchair to increase mobility for the first 6 weeks after surgery. As back surgery and wheelchair use is not covered under the agreement, Authorization for these services needed to be obtained prior to the surgery. The clerk indicated to the patient that they would try to obtain authorization for these services and would let the patient know within the next few days of the result. The clerk prepared an authorization request for these two services to submit to the worker's health benefit plan electronically at the end of the day.
The initial response from worker's health benefit plan indicated they had received the authorization request. There was also a comment that indicated that final results should be available in 2 days.
The next day, final results were received and Authorization was given for all requested services. An Authorization number was quoted that was to be used for billing of these services under the worker's current claim.
To demonstrate how Authorization for Preferred Accommodation is requested and obtained. An Authorization by a Payor is a Payor's commitment to pay for services/products even though a Payor may or may not reserve monies for the approved amount.
This storyboard depicts a delayed response with an initial 'identifier handshake' response followed by final authorization results.
| Auth Init Results Init/Comp, PAccom | |
| Auth Comp Results Init/Comp, PAccom |
Mr. Everyman arrives at the hospital for a pre-operation appointment for a pending hip replacement. Barring complications, Mr. Everyman's total stay will be 7 days. He requests semi-private accommodation.
The hospital administrator submits a query to Mr. Everyman's insurer and receives notification from the insurance carrier that Authorization for Preferred Accommodation is required.
An Authorization request for semi-private accommodation is submitted to Mr. Everyman's insurer. The insurer's adjudicator confirms receipt, issues a claim reference number and a message that final decision would occur in 5 days or less.
After three days, the final results are received from the insurer; semi-private accommodation will be covered in full to a limit of 7-nights accommodation. The assigned claim approval number must always be included in all claim submissions.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of application roles and their relationships in the Version 3 Guide.
An application that requests approval for specific Chiro Physio Services and/or Products before these are rendered.
An approved Authorization Request, Chiro Physo is a Payor's commitment to pay for specified services and/or products, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the accommodation that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive only the Final Authorization Results with no initial response from the Authorization Manager.
An application that requests approval for delivery of healthcare services (e.g. treatment, diagnosis) and/or products (e.g. wheelchair, hearing aid), typically before the services and/or products have been rendered.
An approved Authorization Request, Generic is a Payor's commitment to pay for a service and/or product provided by a generic benefits group, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive only the Final Authorization Results with no initial response from the Authorization Manager.
An application that requests approval for specific Oral Health Services and/or Products before these are rendered.
An approved Authorization Request, Oral Health is a Payor's commitment to pay for specified services and/or products, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive only the Final Authorization Results with no initial response from the Authorization Manager.
An application that requests approval for specific Pharmacy Services and/or Products before these are rendered.
An approved Authorization Request, Pharmacy is a Payor's commitment to pay for specified services and/or products, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the service that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive only the Final Authorization Results with no initial response from the Authorization Manager.
An application that requests approval for specific Physician Services and/or Products before these are rendered.
An approved Authorization Request, Physician is a Payor's commitment to pay for specified services and/or products, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the service that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive only the Final Authorization Results with no initial response from the Authorization Manager.
An application that requests approval for specific Preferred Accomodation (i.e. semi-private, private), typically before the Preferred Accomodation has been used.
An approved Authorization Request, Preferred Accommodation is a Payor's commitment to pay for specified accommodation, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the accommodation that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive only the Final Authorization Results with no initial response from the Authorization Manager.
An application that requests approval for specific Vision Care Services and/or Products before these are rendered.
An approved Authorization Request, Vision Care is a Payor's commitment to pay for specified services and/or products, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive only the Final Authorization Results with no initial response from the Authorization Manager.
An application that requests approval for delivery of healthcare services (e.g. treatment, diagnosis) and/or products (e.g. wheelchair, hearing aid), typically before the services and/or products have been rendered.
An approved Authorization Request is a Payor's commitment to pay for a service and/or product, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive only the Final Authorization Results with no initial response from the Authorization Manager.
An application that requests approval for specific Chiro Physio Services and/or Products before these are rendered
An approved Authorization Request, Chiro Physio is a Payor's commitment to pay for the specified services and/or products, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the accommodation that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive an initial response, which may contain partial results and an indication when the final Authorization Results will be forwarded from the Authorization Manager.
An application that requests approval for delivery of healthcare services (e.g. treatment, diagnosis) and/or products (e.g. wheelchair, hearing aid), typically before the services and/or products have been rendered.
An approved Authorization Request, Generic is a Payor's commitment to pay for a service and/or product, rendered by a generic benefits group, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive an initial response, which may contain partial results and an indication when the final Authorization Results will be forwarded from the Authorization Manager.
An application that requests approval for specific Oral Health Services and/or Products before these are rendered
An approved Authorization Request, Oral Health is a Payor's commitment to pay for the specified services and/or products, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the services and/or products that are authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive an initial response, which may contain partial results and an indication of when the final Authorization Results will be forwarded from the Authorization Manager.
An application that requests approval for specific Pharmacy Services and/or Products before these are rendered.
An approved Authorization Request, Pharmacy is a Payor's commitment to pay for a specified accommodation, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the pharmacy products and/or services that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive an initial response, which may contain partial results and an indication when the final Authorization Results will be forwarded from the Authorization Manager.
An application that requests approval for specific Physician Services and/or Products before these are rendered
An approved Authorization Request, Physician is a Payor's commitment to pay for the specified services and/or products, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the service that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive an initial response, which may contain partial results and an indication of when the final Authorization Results will be forwarded from the Authorization Manager.
An application that requests approval for specific Preferred Accomodation (i.e. semi-private, private), typically before the Preferred Accomodation has been used.
An approved Authorization Request, Preferred Accommodation is a Payor's commitment to pay for a specified accommodation, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the accommodation that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive an initial response, which may contain partial results and an indication when the final Authorization Results will be forwarded from the Authorization Manager.
An application that requests approval for specific Vision Care Services and/or Products before these are rendered
An approved Authorization Request, Vision Care is a Payor's commitment to pay for the specified services and/or products, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the services and/or products that are authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive an initial response, which may contain partial results and an indication of when the final Authorization Results will be forwarded from the Authorization Manager.
An application that requests approval for delivery of healthcare services (e.g. treatment, diagnosis) and/or products (e.g. wheelchair repair, hearing aid), typically before the services and/or products have been rendered.
An approved Authorization Request is a Payor's commitment to pay for a service and/or product, even though a Payor may or may not reserve monies for the approved amount.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
The Authorization Requestor will receive an initial response, which may contain partial results and an indication when the final Authorization Results will be forwarded from the Authorization Manager.
An application that responds to an Authorization Request, Chiro Physio with the final Authorization Results only.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Generic with the final Authorization Results only.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Oral Health with the final Authorization Results only.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Pharmacy with the final Authorization Results only.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Physician with the final Authorization Results only.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Preferred Accommodation with the final Authorization Results only.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Vision Care with the final Authorization Results only.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request with the final Authorization Results only.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Chiro Physio with Final Authorization Results if possible. If Final Authorization Results are not possible, then the Authorization Manager may respond with Initial Authorization Results that can include partial or incomplete processing results and an indication of when the Final Authorization Results will be available.
When the Authorization Manager, Initial/Final Results sends the completed Authorization Results, they act as an Authorization Notifier. This Application Role includes the Notifier Application Role.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Generic with Final Authorization Results if possible. If Final Authorization Results are not possible, then the Authorization Manager may respond with Initial Authorization Results that can include partial or incomplete processing results and an indication of when the Final Authorization Results will be available.
When the Authorization Manager, Initial/Final Results sends the completed Authorization Results, they act as an Authorization Notifier. This Application Role includes the Notifier Application Role.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Oral Health with Final Authorization Results if possible. If Final Authorization Results are not possible, then the Authorization Manager may respond with Initial Authorization Results that can include partial or incomplete processing results and an indication of when the Final Authorization Results will be available.
When the Authorization Manager, Initial/Final Results sends the completed Authorization Results, they act as an Authorization Notifier. This Application Role includes the Notifier Application Role.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Pharmacy with Final Authorization Results if possible. If Final Authorization Results are not possible, then the Authorization Manager may respond with Initial Authorization Results that can include partial or incomplete processing results and an indication of when the Final Authorization Results will be available.
When the Authorization Manager, Initial/Final Results sends the completed Authorization Results, they act as an Authorization Notifier. This Application Role includes the Notifier Application Role.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Physician with Final Authorization Results if possible. If Final Authorization Results are not possible, then the Authorization Manager may respond with Initial Authorization Results that can include partial or incomplete processing results and an indication of when the Final Authorization Results will be available.
When the Authorization Manager, Initial/Final Results sends the completed Authorization Results, they act as an Authorization Notifier. This Application Role includes the Notifier Application Role.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Preferred Accommodation with Final Authorization Results if possible. If Final Authorization Results are not possible, then the Authorization Manager may respond with Initial Authorization Results that can include partial or incomplete processing results and an indication of when the Final Authorization Results will be available.
When the Authorization Manager, Initial/Final Results sends the completed Authorization Results, they act as an Authorization Notifier. This Application Role includes the Notifier Application Role.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request, Vision Care with Final Authorization Results if possible. If Final Authorization Results are not possible, then the Authorization Manager may respond with Initial Authorization Results that can include partial or incomplete processing results and an indication of when the Final Authorization Results will be available.
When the Authorization Manager, Initial/Final Results sends the completed Authorization Results, they act as an Authorization Notifier. This Application Role includes the Notifier Application Role.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application that responds to an Authorization Request with Final Authorization Results if possible. If Final Authorization Results are not possible, then the Authorization Manager may respond with Initial Authorization Results that can include partial or incomplete processing results and an indication of when the Final Authorization Results will be available.
When the Authorization Manager, Initial/Final Results sends the completed Authorization Results, they act as an Authorization Notifier. This Application Role includes the Notifier Application Role.
The Final Authorization Results may grant or deny Authorization for rendering healthcare services or supplying products. If Authorization is denied, the Payor will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, limits such as maximum amount, maximum quantity, timeframes and other limits may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Authorization Manager (Payor).
An application responsible for sending notification of Final Authorization Results to an Authorization Tracker.
An application responsible for sending notification of Final Authorization Results, Chiro Physio to an Authorization Tracker.
An application responsible for sending notification of Final Authorization Results, Generic to an Authorization Tracker.
An application responsible for sending notification of Final Authorization Results, Pharmacy to an Authorization Tracker.
An application responsible for sending notification of Final Authorization Results, Physician to an Authorization Tracker.
An application responsible for sending notification of Final Authorization Results, Preferred Accommodation to an Authorization Tracker.
An application responsible for tracking Authorization Results from an Authorization Notifier.
An example of an Authorization Tracker could be a head office, accountant or a payee.
An application responsible for tracking Authorization Results, Chiro Physio from an Authorization Notifier.
An example of an Authorization Tracker could be a head office, accountant or a payee.
An application responsible for tracking Authorization Results, Generic from an Authorization Notifier.
An example of an Authorization Tracker could be a head office, accountant or a payee.
An application responsible for tracking Authorization Results, Pharmacy from an Authorization Notifier.
An example of an Authorization Tracker could be a head office, accountant or a payee.
An application responsible for tracking Authorization Results, Physician from an Authorization Notifier.
An example of an Authorization Tracker could be a head office, accountant or a payee.
An application responsible for tracking Authorization Results, Preferred Accommodation from an Authorization Notifier.
An example of an Authorization Tracker could be a head office, accountant or a payee.
|
||||||||||||||||||||||
|
For details on the interpretation of this section, see the discussion of trigger events in the Version 3 Guide.
| Type: | State-transition based |
| State Transition: | PaymentRequest (FICR_RM300000UV03) |
A trigger to send an Authorization Request for approval for delivery of healthcare services (e.g., treatment, diagnosis) and/or products (e.g., wheelchair, hearing aid); typically before the services and/or products have been rendered.
An approved Authorization Request is a Adjudicator's commitment to pay for a service and/or product, even though the Adjudicator may or may not reserve monies for the requested amount.
The Provider may or may not actually bill for the service and/or product that is authorized. Therefore, Authorization Requests that are approved typically have expiration dates and limits on their use.
| Type: | Interaction based |
A trigger to send an initial Authorization Results when the Adjudicator has completed an initial preprocessing of the Authorization Request.
Final results will come later (e.g. next day) as an unsolicited result.
The initial results may include preliminary edits such as patient identifier and date validation as well as patient eligibility validation. The initial results may also indicate when the final results may be expected.
| Type: | State-transition based |
| State Transition: | PaymentIntent (FICR_RM310000UV03) |
A trigger to send a completed Authorization Result.
This trigger may be fired close to immediate (i.e., in the same submission/response interaction as the request) or may lag the request by a period of time (perhaps one or more days).
The completed Authorization Results may grant or deny authorization for rendering healthcare services or supplying products. If Authorization is denied, the Adjudicator will not pay for any costs incurred in the delivery of the specified service or product. If the Authorization is granted, the maximum amount that will be paid for the service may be included in the response.
Approved Authorizations represent a commitment to pay for the service and/or product by the Adjudicator.
| Type: |
A trigger that indicated that the Adjudicator has accepted responsibility for the Authorization Nullify Request and will respond with completed results (accept, reject) at a later point (e.g. next day).
| Type: |
A trigger that indicated successful completion of an Authorization Nullify Request. In other words, the request has been nullified.
| Type: | State-transition based |
| State Transition: | InvoiceElementGroup (FICR_RM320000UV01) |
A trigger to send an Authorization Nullify Request.
The response to the request may be accepted or rejected, depending on the ability of the Adjudicator to nullify the request.
| Type: |
A trigger that indicated unsuccessful completion of an Authorization Nullify Request. In other words, the request has NOT been nullified.
| Type: | User request |
A trigger to send an Authorization Query Request to determine the existence and status of an Authorization Request.
For example, a diagnostic facility may wish to confirm that the services to be rendered have previously been authorized by a general practitioner (a pre-condition to payment by an insurance company to a diagnostic facility may be a referral from a general practitioner in the form of an Authorization).
| Type: | Interaction based |
A trigger to send an Authorization Query Response indicating the existence and status of an Authorization Request.
Authorization Query Response may indicate that the Authorization Request processing is not completed; or if completed, will confirm that Authorization was given or will indicate that Authorization is denied.
|
||||||||||||
|
For details on the interpretation of this section, see the description of RMIMs in the Version 3 Guide.
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to submit an Authorization Request by a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
Prior to performing a service or selling a product, the Provider may attempt to obtain authorization to confirm that an Adjudicator will pay for the service(s) and/or product(s).
The 2 core classes referenced in the RMIM are the FinancialTransaction, cloned as the PaymentRequest in the PRP: proposal mood and the InvoiceElement, cloned as the InvoiceElementGroup, InvoiceElementDetail.
The message structure is the same as the Invoice including specification of the Covered Party(Patient), PolicyOrAccount (insurance), FinancialContract, Accident, Health DocumentAttachment and a reference to the service and/or product that requires authorization (through the A_Billable CMET).
| Authorization Request Generic | FICR_HD300100UV02 |
| Authorization Request Pharmacy | FICR_HD300200UV01 |
| Authorization Request Preferred Accommodation | FICR_HD300300UV02 |
| Authorization Request Chiro/Physio | FICR_HD300400UV02 |
| Authorization Request Oral Health | FICR_HD300500UV03 |
| Authorization Request Vision Care | FICR_HD300600UV03 |
| Authorization Request Physician | FICR_HD300700UV03 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to respond to an Authorization Request message submitted by a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
The authorization response will include a list of InvoiceElements that represent billable items that will be accepted by the Adjudicator.
The 2 core classes referenced in the RMIM are the FinancialTransaction, cloned as the PaymentRequest and the InvoiceElement, cloned as the InvoiceElementGroup and InvoiceElementDetail.
The message structure is the same as the Adjudication Results with the details and includes AdjudicatedInvoiceElement acts to specify adjustments to the InvoiceElementDetails that were specified. Limits to the coverage are specified as AdjudicationResultsInformation items (OBS: observations) as pertinent information to the AdjudicationResult.
A positive authorization response (i.e. authorized) may also indicate that the Adjudicator has set aside funds for the subject of the Authorization (e.g. medical procedure).
| Authorization Results Generic | FICR_HD310100UV02 |
| Authorization Results Pharmacy | FICR_HD310200UV01 |
| Authorization Results Preferred Accommodation | FICR_HD310300UV02 |
| Authorization Results Chiro/Physio | FICR_HD310400UV02 |
| Authorization Results Oral Health | FICR_HD310500UV03 |
| Authorization Results Vision Care | FICR_HD310600UV03 |
| Authorization Results Physician | FICR_HD310700UV03 |
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to submit an Authorization Nullify Request from a healthcare product or services Provider (e.g. individual healthcare practitioner, healthcare facility, pharmacy, medical goods and supplies purveyors, etc.) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization and/or their agents).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
The Provider needs to Nullify a previous request to obtain Authorization to perform specified services or supply specified goods.
The core class referenced in the RMIM are the InvoiceElement, cloned as one InvoiceElementGroup.
The message references a group in the Authorization Request.
| Authorization Nullify Request | FICR_HD320100UV02 |
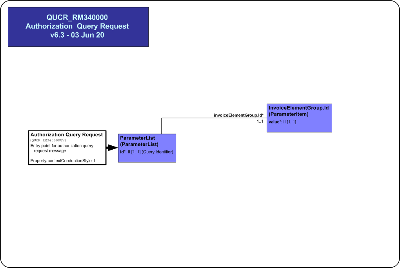
| Parent: | Claims & Reimbursement (FICR_DM000000UV03) |
This model represents a message used to send the Authorization Query Request message from a Provider (e.g. individual practitioner, healthcare facility, medical goods and supplies purveyor) to an Insurance Carrier (e.g. jurisdictional medical services plan, insurance organization, workers compensation organization).
An Insurance Carrier may delegate performance of this function to an Adjudicator (agent of the Insurance Carrier). Subsequent discussions only note Provider and Adjudicator (not Insurance Carrier).
Prior to performing a billable act and invoicing, the Provider may make a query on the status of a Request for authorization to perform specified services or supply specified goods they had previously made.
This query is a single parameter, the Invoice Element root Group identifier, from the Authorization Request being queried.
The Authorization Results message is returned in response to this query.
| Authorization Query Request | QUCR_HD340100UV02 |
|
||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the description of HMDs in the Version 3 Guide.
This message is used to send results of a Chiro Physio Authorization Request to a Provider Application. If the Authorization is approved, then the Adjudicator Application will return either an Authorization Number (AdjudicatedInvoiceElementGroup id) or an individual (AdjudicatorPerson) who is the responsible entity authorizing the items. The authorization status is specified as the AdjudicationResultReason observation value (authorized, not authorized).
This message is used to send results of a generic Authorization Request to a Provider Application. If the Authorization is approved, then the Adjudicator Application will return an Authorization Number (AdjudicatedInvoiceElementGroup id) or an individual (AdjudicatorPerson) who is the responsible entity authorizing the items. The authorization status is specified as the AdjudicationResultReason observation value (authorized, not authorized).
This message is used to send results of a Oral Health Authorization Request to a Provider Application. If the Authorization is approved, then the Adjudicator Application will return either an Authorization Number (AdjudicatedInvoiceElementGroup id) or an individual (AdjudicatorPerson) who is the responsible entity authorizing the items. The authorization status is specified as the AdjudicationResultReason observation value (authorized, not authorized).
This message is used to send results of a Pharmacy Authorization Request to a Provider Application. If the Authorization is approved, then the Adjudicator Application will return either an Authorization Number (AdjudicatedInvoiceElementGroup id) or an individual (AdjudicatorPerson) who is the responsible entity authorizing the items. The authorization status is specified as the AdjudicationResultReason observation value (authorized, not authorized).
This message is used to send results of a Physician Authorization Request to a Provider Application. If the Authorization is approved, then the Adjudicator Application will return either an Authorization Number (AdjudicatedInvoiceElementGroup id) or an individual (AdjudicatorPerson) who is the responsible entity authorizing the items. The authorization status is specified as the AdjudicationResultReason observation value (authorized, not authorized).
This message is used to send results of a Preferred Accomondation Authorization Request to a Provider Application. If the Authorization is approved, then the Adjudicator Application will return either an Authorization Number (AdjudicatedInvoiceElementGroup id) or an individual (AdjudicatorPerson) who is the responsible entity authorizing the items. The authorization status is specified as the AdjudicationResultReason observation value (authorized, not authorized).
This message is used to send results of a Vision Care Authorization Request to a Provider Application. If the Authorization is approved, then the Adjudicator Application will return either an Authorization Number (AdjudicatedInvoiceElementGroup id) or an individual (AdjudicatorPerson) who is the responsible entity authorizing the items. The authorization status is specified as the AdjudicationResultReason observation value (authorized, not authorized).
This message is used to Nullify an Authorization Request previously submitted.
This message can be used to Nullify one InvoiceElementGroup in an Authorization Request.
This message cannot be used to update ancillary information in an Authorization Request that has been submitted. The original request group(s) must be nullified, and a new Authorization Request submitted to the Adjudicator.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
For details on the interpretation of this section, see the definition of Interactions in the Version 3 Guide.
The sender sends an Authorization Results message containing the inital Authorization Results for Chiro Physio services and/or products. Completed results will follow at a later point in time (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Initial Confirmation | FICR_TE310102UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Chiro Physio | FICR_MT310401UV02 |
| Sender | Auth Mgr,Init/Comp Rslts, ChiroPhysio | FICR_AR033004UV02 |
| Receiver | Auth Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR031004UV02 |
The sender sends an Authorization Results message containing the inital Authorization Results for Generic services and/or products. Completed results will follow at a later point in time (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Initial Confirmation | FICR_TE310102UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Generic | FICR_MT310101UV02 |
| Sender | Auth Mgr, Init/Comp Rslts, Gen | FICR_AR033001UV02 |
| Receiver | Auth Rqstr, Init/Comp Rslts, Gen | FICR_AR031001UV02 |
The sender sends an Authorization Results message containing the inital Authorization Results for Oral Health services and/or products. Completed results will follow at a later point in time (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Initial Confirmation | FICR_TE310102UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Oral Health | FICR_MT310501UV03 |
| Sender | Auth Mgr, Init/Comp Rslts, OralHealth | FICR_AR033005UV03 |
| Receiver | Auth Rqstr, Init/Comp Rslts, OralHealth | FICR_AR031005UV03 |
The sender sends an Authorization Results message containing the inital Authorization Results for Pharmacy services and/or products. Completed results will follow at a later point in time (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Initial Confirmation | FICR_TE310102UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Pharmacy | FICR_MT310201UV01 |
The sender sends an Authorization Results message containing the inital Authorization Results for Physician services and/or products. Completed results will follow at a later point in time (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Initial Confirmation | FICR_TE310102UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Physician | FICR_MT310701UV03 |
| Sender | Auth Mgr, Init/Comp Rslts, Physician | FICR_AR033007UV03 |
| Receiver | Auth Rqstr, Init/Comp Rslts, Physician | FICR_AR031007UV03 |
The sender sends an Authorization Results message containing the inital Authorization Results for Preferred Accommodation services and/or products. Completed results will follow at a later point in time (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Initial Confirmation | FICR_TE310102UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Pref Accom | FICR_MT310301UV02 |
| Sender | Auth Mgr, Init/Comp Rslts, PAccom | FICR_AR033003UV02 |
| Receiver | Auth Rqstr, Init/Comp Rslts, PAccom | FICR_AR031003UV02 |
The sender sends an Authorization Results message containing the inital Authorization Results for Vision Care services and/or products. Completed results will follow at a later point in time (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Initial Confirmation | FICR_TE310102UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Vision Care | FICR_MT310601UV03 |
| Sender | Auth Mgr, Init/Comp Rslts, Physician | FICR_AR033007UV03 |
| Receiver | Auth Rqstr, Init/Comp Rslts, Physician | FICR_AR031007UV03 |
The sender sends an Authorization Request message for Chiro Physio services and/or products.
The receiver will provide completed Authorization Results, NOT initial results.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Chiro Physio | FICR_MT300401UV02 |
| Reason | Trigger Event | Interaction |
| Completed Authorization Requests | FICR_TE310101UV02 | FICR_IN310104UV02 |
| Sender | Auth Rqstr, Comp Rslts, ChiroPhysio | FICR_AR030004UV02 |
| Receiver | Auth Mgr, Comp Rslts, ChiroPhysio | FICR_AR032004UV02 |
The sender sends an Authorization Request message for Generic services and/or products.
The receiver will provide completed Authorization Results, NOT initial results.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Generic | FICR_MT300101UV02 |
| Reason | Trigger Event | Interaction |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310101UV02 |
| Sender | Auth Rqstr, Comp Rslts, Gen | FICR_AR030001UV02 |
| Receiver | Auth Mgr, Comp Rslts, Gen | FICR_AR032001UV02 |
The sender sends an Authorization Request message for Oral Health services and/or products.
The receiver will provide completed Authorization Results, NOT initial results.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Oral Health | FICR_MT300501UV03 |
| Reason | Trigger Event | Interaction |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310105UV03 |
| Sender | Auth Rqstr, Comp Rslts, OralHealth | FICR_AR030005UV03 |
| Receiver | Auth Mgr, Comp Rslts, OralHealth | FICR_AR032005UV03 |
The sender sends an Authorization Request message for Pharmacy services and/or products.
The receiver will provide completed Authorization Results, NOT initial results.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Pharmacy | FICR_MT300201UV01 |
The sender sends an Authorization Request message for Physician services and/or products.
The receiver will provide completed Authorization Results, NOT initial results.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Physician | FICR_MT300701UV03 |
| Reason | Trigger Event | Interaction |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310107UV03 |
| Sender | Auth Rqstr, Comp Rslts, Physician | FICR_AR030007UV03 |
| Receiver | Auth Mgr, Comp Rslts, Physician | FICR_AR032007UV03 |
The sender sends an Authorization Request message for Preferred Accommodation services and/or products.
The receiver will provide completed Authorization Results, NOT initial results.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Pref Accom | FICR_MT300301UV02 |
| Reason | Trigger Event | Interaction |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310103UV02 |
| Sender | Auth Rqstr, Comp Rslts, Paccom | FICR_AR030003UV02 |
| Receiver | Auth Mgr, Comp Rslts, Paccom | FICR_AR032003UV02 |
The sender sends an Authorization Request message for Vision Care services and/or products.
The receiver will provide completed Authorization Results, NOT initial results.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Vision Care | FICR_MT300601UV03 |
| Reason | Trigger Event | Interaction |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310106UV03 |
| Sender | Auth Rqstr, Comp Rslts, VisionCare | FICR_AR030006UV03 |
| Receiver | Auth Mgr, Comp Rslts, VisionCare | FICR_AR032006UV03 |
The sender sends an Authorization Request message for Chiro Physio services and/or products.
The receiver will attempt to return completed Authorization Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Chiro Physio | FICR_MT300401UV02 |
| Reason | Trigger Event | Interaction |
| Initial Authorization Results | FICR_TE310102UV02 | FICR_IN310204UV02 |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310304UV02 |
| Sender | Auth Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR031004UV02 |
| Receiver | Auth Mgr,Init/Comp Rslts, ChiroPhysio | FICR_AR033004UV02 |
The sender sends an Authorization Request message for Generic services and/or products.
The receiver will attempt to return completed Authorization Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Generic | FICR_MT300101UV02 |
| Reason | Trigger Event | Interaction |
| Initial Authorization Results | FICR_TE310102UV02 | FICR_IN310201UV02 |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310301UV02 |
| Sender | Auth Rqstr, Init/Comp Rslts, Gen | FICR_AR031001UV02 |
| Receiver | Auth Mgr, Init/Comp Rslts, Gen | FICR_AR033001UV02 |
The sender sends an Authorization Request message for Oral Health services and/or products.
The receiver will attempt to return completed Authorization Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Oral Health | FICR_MT300501UV03 |
| Reason | Trigger Event | Interaction |
| Initial Authorization Results | FICR_TE310102UV02 | FICR_IN310205UV03 |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310305UV03 |
| Sender | Auth Rqstr, Init/Comp Rslts, OralHealth | FICR_AR031005UV03 |
| Receiver | Auth Mgr, Init/Comp Rslts, OralHealth | FICR_AR033005UV03 |
The sender sends an Authorization Request message for Pharmacy services and/or products.
The receiver will attempt to return completed Authorization Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Pharmacy | FICR_MT300201UV01 |
The sender sends an Authorization Request message for Physician services and/or products.
The receiver will attempt to return completed Authorization Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Physician | FICR_MT300701UV03 |
| Reason | Trigger Event | Interaction |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310207UV03 |
| Initial Authorization Results | FICR_TE310102UV02 | FICR_IN310207UV03 |
| Sender | Auth Rqstr, Init/Comp Rslts, Physician | FICR_AR031007UV03 |
| Receiver | Auth Mgr, Init/Comp Rslts, Physician | FICR_AR033007UV03 |
The sender sends an Authorization Request message for Preferred Accommodation services and/or products.
The receiver will attempt to return completed Authorization Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Pref Accom | FICR_MT300301UV02 |
| Reason | Trigger Event | Interaction |
| Initial Authorization Results | FICR_TE310102UV02 | FICR_IN310203UV02 |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310303UV02 |
| Sender | Auth Rqstr, Init/Comp Rslts, PAccom | FICR_AR031003UV02 |
| Receiver | Auth Mgr, Init/Comp Rslts, PAccom | FICR_AR033003UV02 |
The sender sends an Authorization Request message for Vision Care services and/or products.
The receiver will attempt to return completed Authorization Results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Request | FICR_TE300101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Activate Vision Care | FICR_MT300601UV03 |
| Reason | Trigger Event | Interaction |
| Completed Authorization Results | FICR_TE310101UV02 | FICR_IN310306UV03 |
| Initial Authorization Results | FICR_TE310102UV02 | FICR_IN310306UV03 |
| Sender | Auth Rqstr, Init/Comp Rslts, VisionCare | FICR_AR031006UV03 |
| Receiver | Auth Mgr, Init/Comp Rslts, VisionCare | FICR_AR033006UV03 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Chiro Physio services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Chiro Physio | FICR_MT310401UV02 |
| Sender | Auth Mgr, Comp Rslts, ChiroPhysio | FICR_AR032004UV02 |
| Receiver | Auth Rqstr, Comp Rslts, ChiroPhysio | FICR_AR030004UV02 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Generic services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Generic | FICR_MT310101UV02 |
| Sender | Auth Mgr, Comp Rslts, Gen | FICR_AR032001UV02 |
| Receiver | Auth Rqstr, Comp Rslts, Gen | FICR_AR030001UV02 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Oral Health services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Oral Health | FICR_MT310501UV03 |
| Sender | Auth Mgr, Comp Rslts, OralHealth | FICR_AR032005UV03 |
| Receiver | Auth Rqstr, Comp Rslts, OralHealth | FICR_AR030005UV03 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Pharmacy services and/or products.
This notification follows on initial results sent previously.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Pharmacy | FICR_MT310201UV01 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Physician services and/or products.
This notification follows on initial results sent previously.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Physician | FICR_MT310701UV03 |
| Sender | Auth Mgr, Comp Rslts, Physician | FICR_AR032007UV03 |
| Receiver | Auth Rqstr, Comp Rslts, Physician | FICR_AR030007UV03 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Preferred Accommodation services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Pref Accom | FICR_MT310301UV02 |
| Sender | Auth Mgr, Comp Rslts, Paccom | FICR_AR032003UV02 |
| Receiver | Auth Rqstr, Comp Rslts, Paccom | FICR_AR030003UV02 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Vision Care services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Vision Care | FICR_MT310601UV03 |
| Sender | Auth Mgr, Comp Rslts, VisionCare | FICR_AR032006UV03 |
| Receiver | Auth Rqstr, Comp Rslts, VisionCare | FICR_AR030006UV03 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Chiro Physio services and/or products.
This notification follows on initial results sent previously.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Chiro Physio | FICR_MT310401UV02 |
| Sender | Auth Mgr,Init/Comp Rslts, ChiroPhysio | FICR_AR033004UV02 |
| Receiver | Auth Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR031004UV02 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Generic services and/or products.
This notification follows on initial results sent previously.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Generic | FICR_MT310101UV02 |
| Sender | Auth Mgr, Init/Comp Rslts, Gen | FICR_AR033001UV02 |
| Receiver | Auth Rqstr, Init/Comp Rslts, Gen | FICR_AR031001UV02 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Oral Health services and/or products.
This notification follows on initial results sent previously.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Oral Health | FICR_MT310501UV03 |
| Sender | Auth Mgr, Init/Comp Rslts, OralHealth | FICR_AR033005UV03 |
| Receiver | Auth Rqstr, Init/Comp Rslts, OralHealth | FICR_AR031005UV03 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Pharmacy services and/or products.
This notification follows on initial results sent previously.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Pharmacy | FICR_MT310201UV01 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for PhysicianApplication Level Acknowledgement services and/or products.
This notification follows on initial results sent previously.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Physician | FICR_MT310701UV03 |
| Sender | Auth Mgr, Init/Comp Rslts, Physician | FICR_AR033007UV03 |
| Receiver | Auth Rqstr, Init/Comp Rslts, Physician | FICR_AR031007UV03 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Preferred Accommodation services and/or products.
This notification follows on initial results sent previously.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Pref Accom | FICR_MT310301UV02 |
| Sender | Auth Mgr, Init/Comp Rslts, PAccom | FICR_AR033003UV02 |
| Receiver | Auth Rqstr, Init/Comp Rslts, PAccom | FICR_AR031003UV02 |
The sender sends an Authorization Results message containing the completed results of an Authorization Request for Vision Care services and/or products.
This notification follows on initial results sent previously.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Complete Notification | FICR_TE310101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Complete Vision Care | FICR_MT310601UV03 |
| Sender | Auth Mgr, Init/Comp Rslts, VisionCare | FICR_AR033006UV03 |
| Receiver | Auth Rqstr, Init/Comp Rslts, VisionCare | FICR_AR031006UV03 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Chiro Physio services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Comp Rslts, ChiroPhysio | FICR_AR030004UV02 |
| Receiver | Auth Mgr, Comp Rslts, ChiroPhysio | FICR_AR032004UV02 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Generic services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Comp Rslts, Gen | FICR_AR030001UV02 |
| Receiver | Auth Mgr, Comp Rslts, Gen | FICR_AR032001UV02 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Oral Health services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Comp Rslts, OralHealth | FICR_AR030005UV03 |
| Receiver | Auth Mgr, Comp Rslts, OralHealth | FICR_AR032005UV03 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Pharmacy services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Physician services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Comp Rslts, Physician | FICR_AR030007UV03 |
| Receiver | Auth Mgr, Comp Rslts, Physician | FICR_AR032007UV03 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Preferred Accommodation services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Comp Rslts, Paccom | FICR_AR030003UV02 |
| Receiver | Auth Mgr, Comp Rslts, Paccom | FICR_AR032003UV02 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Vision Care services and/or products.
The receiver will provide completed nullify results only. The receiver does NOT return an initial response.
Nullify results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Comp Rslts, VisionCare | FICR_AR030006UV03 |
| Receiver | Auth Mgr, Comp Rslts, VisionCare | FICR_AR032006UV03 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Chiro Physio services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Init/Comp Rslts, ChiroPhysio | FICR_AR031004UV02 |
| Receiver | Auth Mgr,Init/Comp Rslts, ChiroPhysio | FICR_AR033004UV02 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Generic services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Init/Comp Rslts, Gen | FICR_AR031001UV02 |
| Receiver | Auth Mgr, Init/Comp Rslts, Gen | FICR_AR033001UV02 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Oral Health services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Init/Comp Rslts, OralHealth | FICR_AR031005UV03 |
| Receiver | Auth Mgr, Init/Comp Rslts, OralHealth | FICR_AR033005UV03 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Pharmacy services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Physician services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Init/Comp Rslts, Physician | FICR_AR031007UV03 |
| Receiver | Auth Mgr, Init/Comp Rslts, Physician | FICR_AR033007UV03 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Preferred Accommodation services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Init/Comp Rslts, PAccom | FICR_AR031003UV02 |
| Receiver | Auth Mgr, Init/Comp Rslts, PAccom | FICR_AR033003UV02 |
The sender sends an Authorization Nullify Request message to request the nullification of a previously submitted Authorization Request for Vision Care services and/or products.
The receiver will attempt to return completed nullify results, but where this is not possible, initial results will be returned, with the completed results to be sent unsolicited to the sender at a later point (e.g. next day).
The completed results indicate that the receiver was successful or not in nullifying the Authorization Request.
| Trigger Event | Authorization Nullify Request | FICR_TE320101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Trigger Event Control Act | MCAI_MT700201UV01 |
| Message Type | Authorization Event Nullify Request | FICR_MT320101UV02 |
| Sender | Auth Rqstr, Init/Comp Rslts, VisionCare | FICR_AR031006UV03 |
| Receiver | Auth Mgr, Init/Comp Rslts, VisionCare | FICR_AR033006UV03 |
The sender sends an Authorization Query message to determine the status of a previously submitted Authorization Request for Chiro Physio services and/or products.
Query response uses the Authorization Results message.
| Trigger Event | Authorization Query Request | QUCR_TE340101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Authorization Event Query Request | QUCR_MT340101UV02 |
| Reason | Trigger Event | Interaction |
| Authorization Query Response | QUCR_TE350101UV02 | QUCR_IN350104UV02 |
| Sender | Auth Rqstr, Comp Rslts, ChiroPhysio | FICR_AR030004UV02 |
| Receiver | Auth Mgr, Comp Rslts, ChiroPhysio | FICR_AR032004UV02 |
The sender sends an Authorization Query message to determine the status of a previously submitted Authorization Request for Generic services and/or products.
Query response uses the Authorization Results message.
| Trigger Event | Authorization Query Request | QUCR_TE340101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Authorization Event Query Request | QUCR_MT340101UV02 |
| Reason | Trigger Event | Interaction |
| Authorization Query Response | QUCR_TE350101UV02 | QUCR_IN350101UV02 |
| Sender | Auth Rqstr, Comp Rslts, Gen | FICR_AR030001UV02 |
| Receiver | Auth Mgr, Comp Rslts, Gen | FICR_AR032001UV02 |
The sender sends an Authorization Query message to determine the status of a previously submitted Authorization Request for Pharmacy services and/or products.
Query response uses the Authorization Results message.
| Trigger Event | Authorization Query Request | QUCR_TE340101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Authorization Event Query Request | QUCR_MT340101UV02 |
| Reason | Trigger Event | Interaction |
| Authorization Query Response | QUCR_TE350101UV02 | QUCR_IN350102UV01 |
The sender sends an Authorization Query message to determine the status of a previously submitted Authorization Request for Physician services and/or products.
Query response uses the Authorization Results message.
| Trigger Event | Authorization Query Request | QUCR_TE340101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Authorization Event Query Request | QUCR_MT340101UV02 |
| Reason | Trigger Event | Interaction |
| Authorization Query Response | QUCR_TE350101UV02 | QUCR_IN350107UV01 |
The sender sends an Authorization Query message to determine the status of a previously submitted Authorization Request for Preferred Accommodation services and/or products.
Query response uses the Authorization Results message.
| Trigger Event | Authorization Query Request | QUCR_TE340101UV02 |
| Transmission Wrapper | Send Message Payload | MCCI_MT000100UV01 |
| Control Act Wrapper | Query Control Act Request : Parameter List | QUQI_MT020001UV01 |
| Query Definition | Authorization Event Query Request | QUCR_MT340101UV02 |
| Reason | Trigger Event | Interaction |
| Authorization Query Response | QUCR_TE350101UV02 | QUCR_IN350103UV02 |
| Sender | Auth Rqstr, Comp Rslts, Paccom | FICR_AR030003UV02 |
| Receiver | Auth Mgr, Comp Rslts, Paccom | FICR_AR032003UV02 |
The sender sends an Authorization Results message containing the processing status (e.g. active, complete) and/or results of an Authorization Request for Chiro Physio services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Query Response | QUCR_TE350101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Authorization Event Activate Chiro Physio | FICR_MT300401UV02 |
| Sender | Auth Mgr, Comp Rslts, ChiroPhysio | FICR_AR032004UV02 |
| Receiver | Auth Rqstr, Comp Rslts, ChiroPhysio | FICR_AR030004UV02 |
The sender sends an Authorization Results message containing the processing status (e.g. active, complete) and/or results of an Authorization Request for Generic services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Query Response | QUCR_TE350101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Authorization Event Complete Generic | FICR_MT310101UV02 |
| Sender | Auth Mgr, Comp Rslts, Gen | FICR_AR032001UV02 |
| Receiver | Auth Rqstr, Comp Rslts, Gen | FICR_AR030001UV02 |
The sender sends an Authorization Results message containing the processing status (e.g. active, complete) and/or results of an Authorization Request for Pharmacy services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Query Response | QUCR_TE350101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Authorization Event Activate Pharmacy | FICR_MT300201UV01 |
The sender sends an Authorization Results message containing the processing status (e.g. active, complete) and/or results of an Authorization Request for Physician services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Query Response | QUCR_TE350101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Authorization Event Activate Physician | FICR_MT300701UV03 |
The sender sends an Authorization Results message containing the processing status (e.g. active, complete) and/or results of an Authorization Request for Preferred Accommodation services and/or products.
Authorization Results indicate approval or disapproval to render the requested services and/or products, as well as the extent to which the Adjudicator will pay for those services and/or products.
| Trigger Event | Authorization Query Response | QUCR_TE350101UV02 |
| Transmission Wrapper | Application Level Acknowledgement | MCCI_MT000300UV01 |
| Control Act Wrapper | Query Control Act Response / Acknowledgement | QUQI_MT120001UV01 |
| Query Definition | Authorization Event Activate Pref Accom | FICR_MT300301UV02 |
| Sender | Auth Mgr, Comp Rslts, Paccom | FICR_AR032003UV02 |
| Receiver | Auth Rqstr, Comp Rslts, Paccom | FICR_AR030003UV02 |
| Return to top of page |

